High Blood Pressure: Misdiagnosed and Mistreated.
How and why millions are taking pills they may not need.

Background
As a medical student one of the most basic things we are taught about is high blood pressure, or hypertension.
Hypertension is blood pressure that is measured to be consistently high, as compared to a consensus range that is considered to be “normal.”
In the United States, normal blood pressure is under 120/80. 120 refers to systolic blood pressure, and 80 refers to diastolic.
I say consensus, because these normal ranges are not determined by some objective valid standard. In part, this is because hypertension is not a disease in and of itself.
Hypertension is an indicator that your body is at dis-ease.
Needless to say, hypertension is one of the most aggressively ‘treated’ clinical findings in medicine. In part, because it tends to co-occur with many other markers of chronic illness which can have long-term consequences.
Over a year ago I wrote a two-part series exploring the nature of the circulatory system, what blood pressure is, and what it’s derangements indicate.
This article is not about that.
This article is about how high blood pressure is over-diagnosed, and most importantly…mistreated.
Over-Diagnosing Hypertension
When I began my medical education, the definition of “hypertension” was different than what it is today. Back then, systolic blood pressure between 130-139 was considered “elevated” or pre-hypertensive.
Nowadays, if your systolic blood pressure is even 1 mmHg above normal, this is considered “elevated.”
As you can, the definition of hypertension varies by geography and the organization which develops these consensus criteria.
So, if a young and otherwise healthy adult walks into a doctor’s office in the US with a BP of 135/80…you would be diagnosed with Stage 1 Hypertension. However, if you happen to live in Europe…you may just walk out of there with “high-normal blood pressure” and a warning.
The trend of lowering the cut-off values for diagnosing hypertension has been ongoing for decades.
To complement this, the trend of treating blood pressure with prescription drugs has been increasing. In more recent years, clinical trials have been conducted to justify a “multi-modal” approach. What that usually results in is a treatment regimen in which the “multi” refers to multiple different prescription drugs.
Obviously, the lowering of these diagnostic thresholds will have higher impact on the younger and healthier among us. Which may seem like a great strategy, because you would want to “nip the problem in the bud,” so to speak.
But, there is yet another problem.
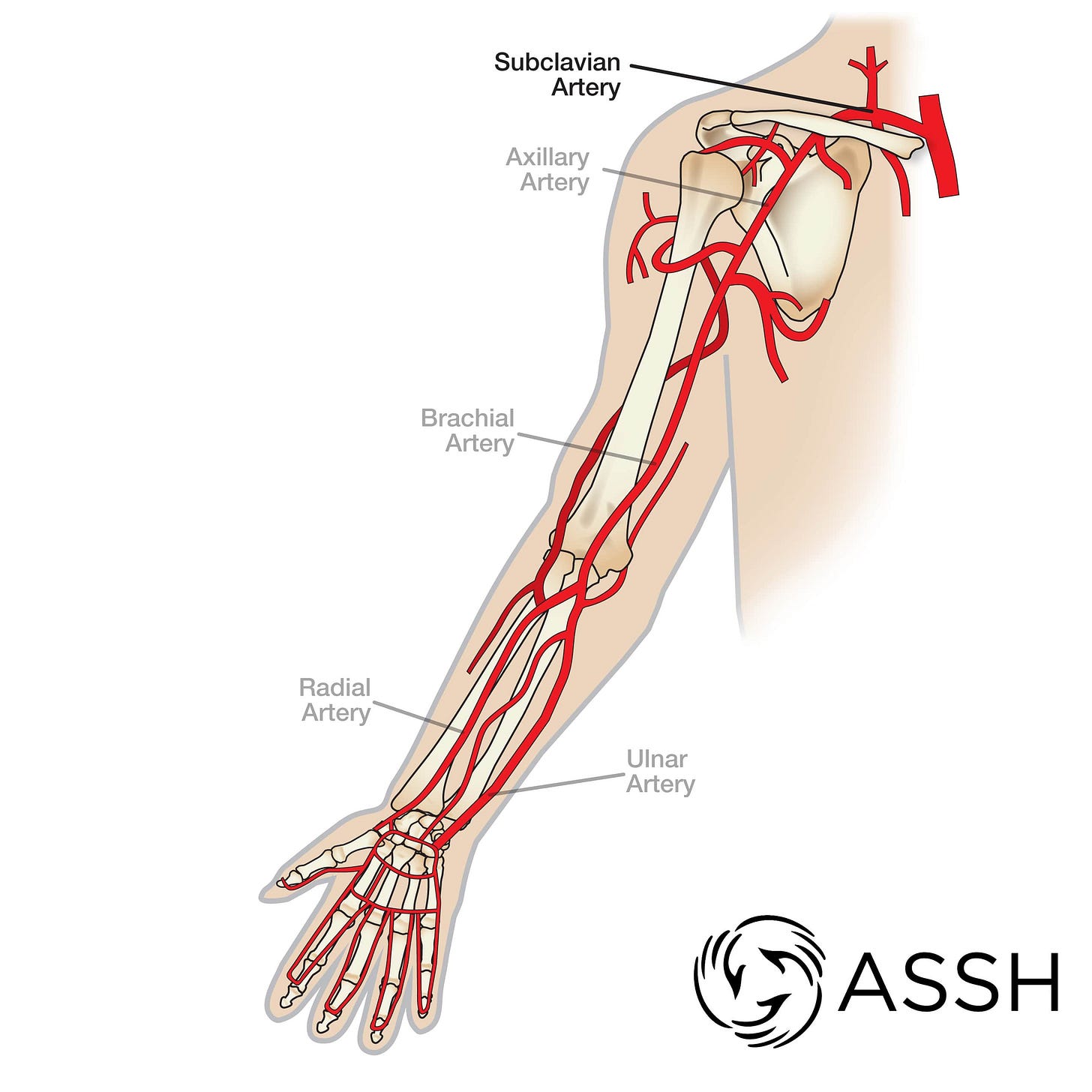
When blood pressure is measured, it is measured in the arm. Specifically, the brachial artery. This is not because we are worried about complications to the arm or your hands. No.
We measure the brachial artery pressure because it is one of the closest arteries to the Aorta (the large artery originating from the heart) that we can also measure non-invasively.
Thus, the pressure in the brachial artery is supposed to be an indicator of the pressure in the Aorta. The aortic pressure is what really matters. Because, it is from the aorta that we get direct branches to the heart (coronary arteries), brain (carotid arteries) and kidneys (renal arteries). These are the organs we are most concerned about when discussing chronic hypertension.
Why am I differentiating this?
Because, we cannot simply assume that the pressure we measure in the arm is the same as the pressure in the aorta! Especially when it’s an artery in a part of the body we use almost every waking minute.
In fact, when we look at the pressure measured from inside the arteries themselves, we can see that as you move from the Aorta to the arm…the pressure in the vessels increase.
Which means that a brachial artery pressure of 135/80 does not mean the aorta has this much pressure.
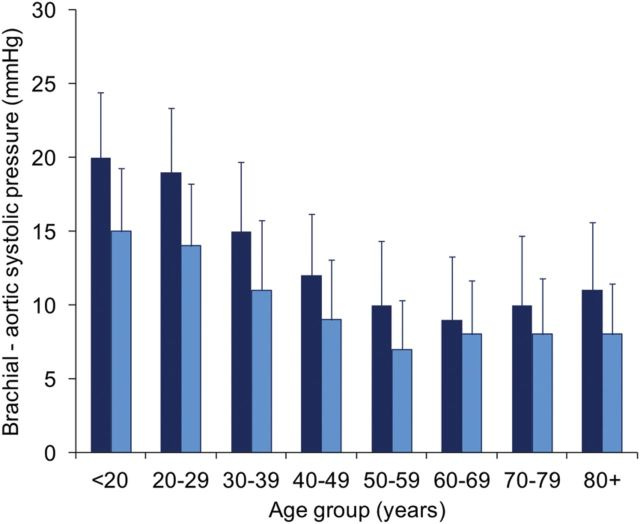
To add insult to injury, the younger you are…the greater the difference between the aortic pressure and the brachial artery pressure.
In the above graph you can see that in young adults (males more than females) the difference between the brachial and aortic systolic pressure is anywhere from 10 to 25 mmHg.
That is enough of a difference to move an otherwise healthy young adult into the “hypertensive” category.
Mis-Treating Hypertension
When it comes to treating hypertension, most family doctors and especially cardiologists are practically evangelical.
Their reasoning goes something like this.
Hypertension causes vascular remodeling that puts stress on and ultimately deprives our organs of blood. The most common organ that is monitored for this strategy is the kidney, and markers of kidney function.
I think they have a point. Chronically elevated blood-pressure is an indicator of dis-ease. The factors which lead to elevated blood pressure are only exacerbated by hypertension itself…which ultimately leads to organ dysfunction.
But, this is where I depart from your standard MD.
I do not think simply forcing blood pressure to go down by using a cocktail of drugs actually helps patients. In fact, as you get older and/or more frail…these drugs can lead to catastrophic outcomes.
If you want to explore some of the articles I’ve reviewed looking at the benefits of simply treating the number (elevated blood pressure), you can do so here:
Fundamentally, hypertension is not a disease. Hypertension is a sign. It’s a sign of other things going on in your body and bloodstream that is requiring the circulatory system to respond by elevating blood pressure.
Unless you uncover and treat the underlying problems…simply lowering blood pressure will not help.
There are many causes of elevated blood pressure. Sometimes the causes are within the bloodstream. Such as electrolyte imbalance, charge insulation, or high viscosity. Other times, high blood pressure is due to disease within specific organs or glands, such as the thyroid gland or the kidneys.
In my opinion, you are far better off focusing on the following than simply taking drugs:
Be active!
Grounding/earthing.
Adequate sunlight. Corollary, avoid artificial lighting - it confuses the body.
Consume more salts. Real salts. Not the big-box store NaCl table salt.
Do things which relieve stress for you, whatever they are.
Eat well.
If you’d like to read about a case study in my approach to curing high blood pressure without medications:







This is so true. I actually found a study from 2017, I’ll have to fish it out. It made it very clear that when checking your blood pressure, you need to be lying down and wait 25 minutes before testing.
Most people get the instruction from their doctors to sit up straight and wait three minutes. And when you’re in the doctors office, you barely have the proper time.
So there’s probably at least 50% over diagnosis of high blood pressure that doesn’t exist just based off of the improper testing
And then add to the fact that the thresholds keep going lower and lower. No 70 year-old should be shooting for 120/70. As we get older, we need higher blood pressure to function. Blood pressure is also upwards of 10 mm/HG higher in the winter. If your body is cold, it will raise the blood pressure.
There is a lot of evidence to show that the majority of high blood pressure is caused by extra weight on the body. And in my case in specific, losing 30 pounds returned my blood pressure to a totally normal range. So since then I have looked at several studies that show fasting and weight loss can reduce blood pressure in almost 100% of cases back to healthy ranges. This leads me to believe That the majority of people should just lose some weight. lol. No drugs required. I didn’t say it was “easy” but it comes with a lot of positive side effects, unlike the drugs.