Understanding Blood Flow & Pressure | Part 2
Now that we have discussed the essence of blood and flow, we explore hypertension, if and how to treat it.

Moving On…
In Part 1 we covered a foundational set of ideas about the nature of blood and circulation, including:
What blood is.
How blood flows.
Why blood flows.
If you haven’t yet read Part 1 of this series, I would highly recommend that you stop right here, and read it first.
In this article we will dive into one of the most commonly diagnosed and treated illnesses in the modern era: high blood pressure or hypertension.
We will answer:
What is blood pressure?
Why is high blood pressure bad?
Does normalizing blood pressure improve health?
What is the best way to reduce blood pressure?
Blood Pressure
First, it’s important to understand what blood pressure is.
When we discuss ‘blood pressure,’ we refer to the force that the blood exerts on artery walls. As we know from Newton’s third law of motion, as the blood exerts a force on the artery, so too does the artery exert a force on the blood.
This reciprocal interaction between blood vessel and wall results in motion of the blood. If the arteries just kept expanding as a result of blood moving into the vessel…then there would be no force causing the blood to move along the tube.
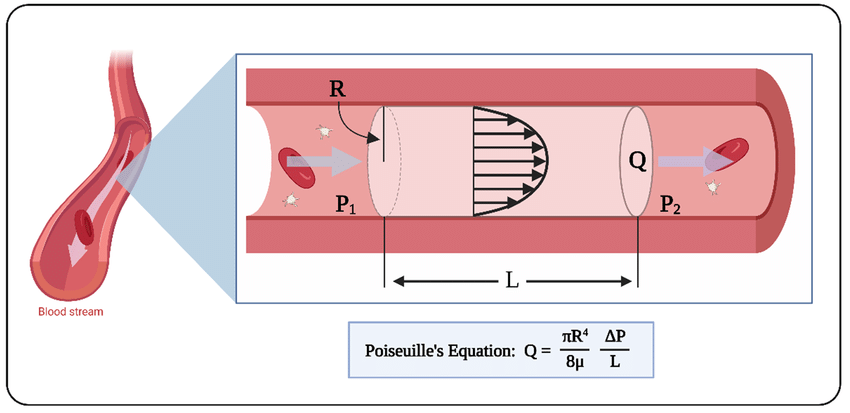
We refer back to the image in Part 1, demonstrating the relationship between flow, pressure, and viscosity as captured by Poiseuille.
What is important to recognize is that the speed of blood flow is directly related to the difference in the pressure between two points in a vessel.
But, the blood does not exert a force on a static vessel. The vasculature of the whole body is malleable and actively controlled. Our body has evolved to release vaso-active substances which alter the tension within the artery wall to regulate flow.
For example, when you eat food…the digestive tract will respond by dilating the arteries that feed the gut…which reduces the resistance along this path…and enables the flow of larger quantities of blood. By making a path of ‘lesser resistance,’ the body controls how much blood flows to a target organ.
How Blood Pressure Is Measured
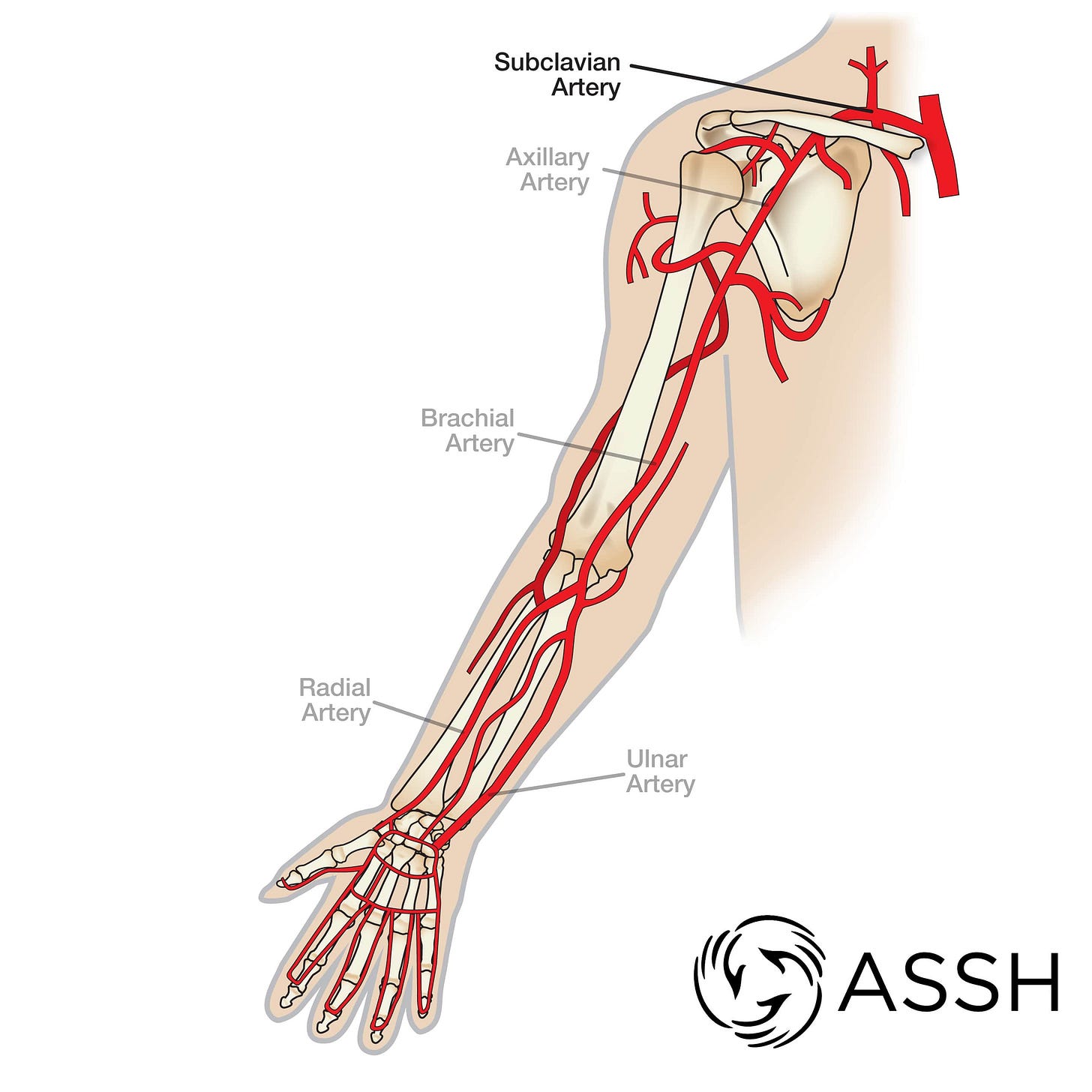
Typically, blood pressure is measured along the arm - as anyone who’s been to a family doctor or emergency department knows. The closer to the heart, the more ‘reliable’ the measurement.
In reality, when your blood pressure is measured…it is actually a measure of the pressure in the brachial artery.
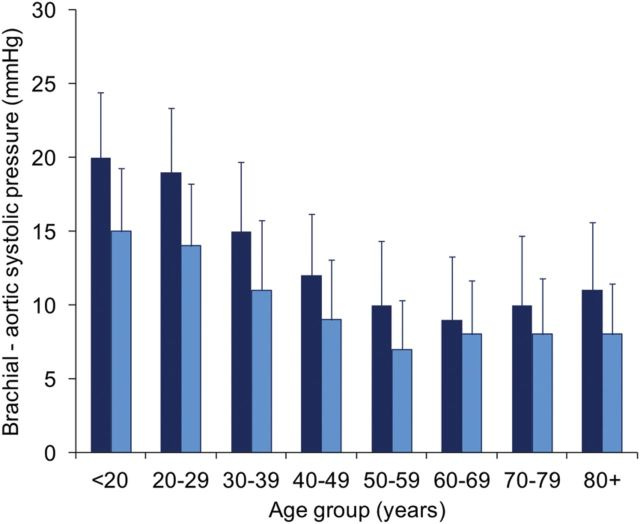
There are several problems with using the brachial artery as an indicator of cardiovascular fitness. First, the brachial artery often overestimates systolic blood pressure, sometimes by up to 40 mmHg!
As it turns out, the younger you are the greater the mismatch between blood pressure in the arm, and central blood pressure coming out of the heart.
This is a bit of a digression, but suffice it to say both the method by which we measure blood pressure and the thresholds we use to assess overall health are not as concrete as your doctor or the American Heart Association may make it sound.
Furthermore, the thresholds use to define hypertension have been changing over the last 20 years. In fact, when I started medical school what I was taught as “stage 1 hypertension” had shifted by the time I had finished my training.
As you can see, the US is a bit of an outlier (since new guidelines from 2017) when it comes to definitions of “hypertension.” In Europe, if you have a systolic BP between 120-130, this is considered normal. In the US, this is considered “elevated.”
More importantly, if you are European and your diastolic BP can be up to 85 mmHg and you are considered “normal.” In the US, however, this is considered Stage 1 Hypertension. It should be noted that these diastolic thresholds are used to justify treatment of “high blood pressure” in otherwise healthy young adults.
As we noted, the younger population tend to have higher blood pressure in their arms.
As you can see from the chart above, the European guidelines agree with the International Society of Hypertension.
Is High Blood Pressure Bad?
Short answer: It can be.
And, it probably is for the vast majority of people who have chronically elevated blood pressure.
Why?
In our modern time, most people have chronically elevated blood pressure because of underlying metabolic dysfunction. All of the common chronic illnesses that people have, including: diabetes, obesity, autoimmune and inflammatory conditions…are caused by the same things which can lead to high blood pressure.
What I didn’t mention is cardiovascular disease. That is because it is not only cardiovascular ‘disease’ which causes high blood pressure. It is an unfit cardiovascular system.
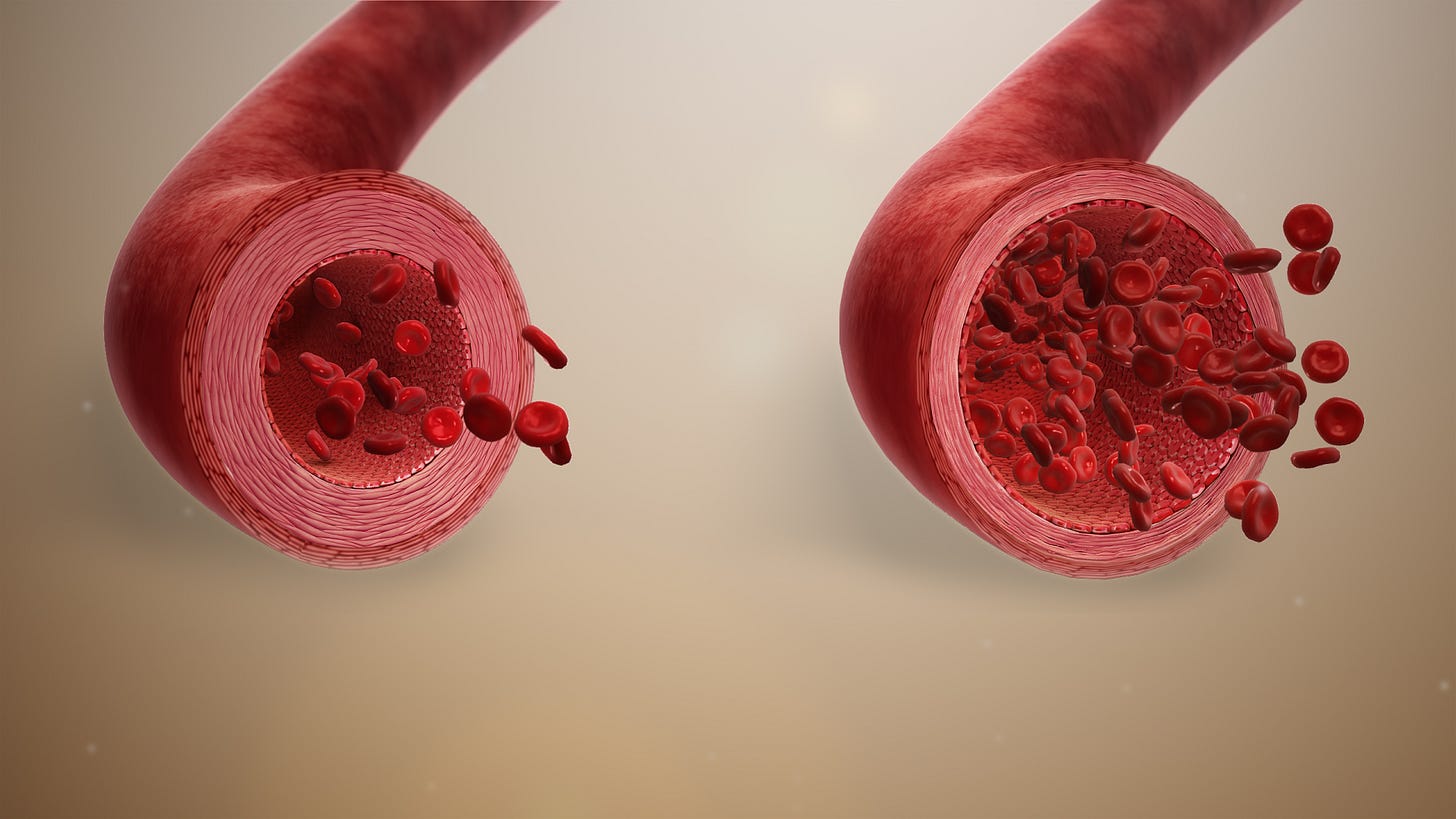
Just like your organs will regulate how much blood reaches them, your heart and arteries must be healthy enough to effectively supply blood where it is needed…without undue stress upon itself. People who live a sedentary life, do not put the heart and blood vessels under stress.
Going for a sprint, swimming and lifting weights do not only work out your muscles and joints.
Your heart and blood vessels expand and contract to the demands of your body, just like your muscles. In doing so, they improve and maintain what can be thought of as circulatory flexibility. Same goes for your lungs.
Two conditions are necessary for healthy blood pressure & heart rate:
Optimal conditioning of your end-organs
including: muscles, kidneys, stomach, liver, brain & skin
Optimal conditioning of your cardiovascular system
Despite what the mainstream medical paradigm will tell you, you cannot simply force your blood vessels to dilate for the purpose of reducing a number - i.e. blood pressure.
Your blood pressure is high for a reason. Unless you address that reason, you will not prevent the damage it is doing to your body.
Worse yet, by forcing your blood vessels into a state they do not wish to be in…you can add additional problems to your health.
Let’s dig further into the literature.
Does Normalizing Blood Pressure Improve Health?
To answer this question, we will look through the findings of two major studies. One published in 2013, and another in 2022.
Both of these studies wanted to explore the relationship between lifestyle changes, medication and health outcomes.
The first study from Brown et al (2013) aimed to assess the impact of physical activity and medication on blood pressure and all-cause mortality. For this observational study consisting of over 10,000 people…the analysis was grouped into multiple categories, all of which included a sub-category of “active” or “inactive”:
On medication with controlled blood pressure
On medication with uncontrolled blood pressure
Not on medication with uncontrolled blood pressure
Normotensive: i.e. not on medication and normal blood pressure
Curves A-H
A: normotensive + active
B: normotensive + inactive
C: treated + active + controlled
D: untreated + active + uncontrolled
E: treated + inactive + controlled
F: untreated + inactive + uncontrolled
G: treated + active + uncontrolled
H: treated + inactive + uncontrolled
There are some very important observations to be made from this study.
Even if your blood pressure is normal, physical activity improves mortality as demonstrated by the difference between curves A and B
It is obviously bad for your health to be chronically hypertensive as demonstrated by the huge gap between A/B and all other curves.
Although the authors report a “significant difference” between curves C and D…upon closer inspection, you can see that they are almost identical just until after 200 months. In fact, curves C and D are closer to one another along their entire length than any other curve on that graph.
What I want to highlight from this observation is the critical importance of being active. This is the common attribute between curves C and D.
Whatever difference exists between C and D (which I’m sure, ultimately there is a difference)…the impact is likely not nearly as significant as being active.