Understanding Blood Flow & Pressure | Part 1
To get a grasp on hypertension, why it happens, and how to treat it...we need to completely reframe our understanding of the circulatory system.

Circulatory Physiology
The biophysics of the circulatory system has fascinated me since before medical school. It may be that early exposure to biophysics planted a seed of curiosity that continues to flourish to this day.
Circulation is far more fascinating than the mainstream medical paradigm lets on.
Even for radiologists, it is one of the few systems of the body which we need to assess in 4 dimensions - that is to say, across time.
Most of radiology takes pictures of the body which are snapshots in time. Cardiac and vascular imaging on the other hand, require assessment of function across time. This is why we employ ultrasound and flow-related imaging techniques. This is a good starting point for diagnosis. But, it is nowhere near enough.
The circulatory system is a hyper-dynamic and infinitely complex interplay of Newtonian biomechanical factors, organ function, electrophysiology, and light signaling.
Now, I could spend precious writing real-estate going over the bunk model of circulation that is taught to doctors…or, we could dive right into re-building a more robust understanding.
I’m going to go with the latter, and I hope in the process you will see why it is the superior framework. We will discuss the following:
What is blood?
How does blood flow?
Why does blood flow?
In Part 2 of this series, we will discuss implications for how and why people develop high blood pressure, and how this robust understanding informs the most effective way to treat hypertension.
What Is Blood?
If you want to understand why something is, it would be helpful to first understand what something is.
By all estimates, the majority of blood is water. However, it isn’t simply water with other substances floating in it. When you cut yourself, you don’t see water flowing out. You see a thinner, albeit gel-like suspension. This is because the water is adherent to biological matter. Water has a charge, and biological matter also has a charge. Charges attract and repel depending on their polarity.
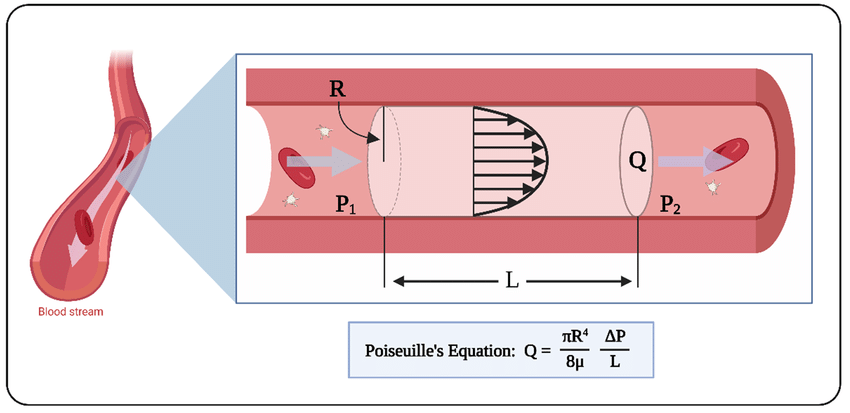
Understanding this in conjunction with the classical Poiseuille’s Law of laminar flow is of utmost importance:
Poiseuille’s equation tells us the relationship between flow of a fluid (Q) with viscosity (µ), as it relates to the difference in pressure (ΔP) across a tube of length (L) and radius (R).
All of these factors are important to understand, as they are modifiable. You could argue that the length of the circulatory system is relatively constant, and as far as I am concerned it is not important for us to debate this point.
What is important to understand is the role of viscosity, flow demand, and radius. The radius of blood vessels change all the time in response to certain stimuli - i.e. vasodilation and vasoconstriction.
But, I digress…
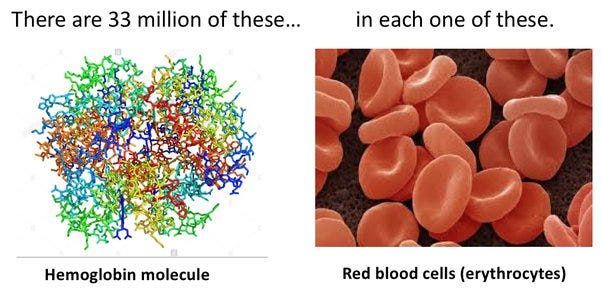
You may have notice there is another major component of blood - erythrocytes.
Erythrocytes are red blood cells (RBCs). RBCs carry hemoglobin. Hemoglobin is what is traditionally taught as being the oxygen-carrier in blood. Which is true. But, there is more to this picture.
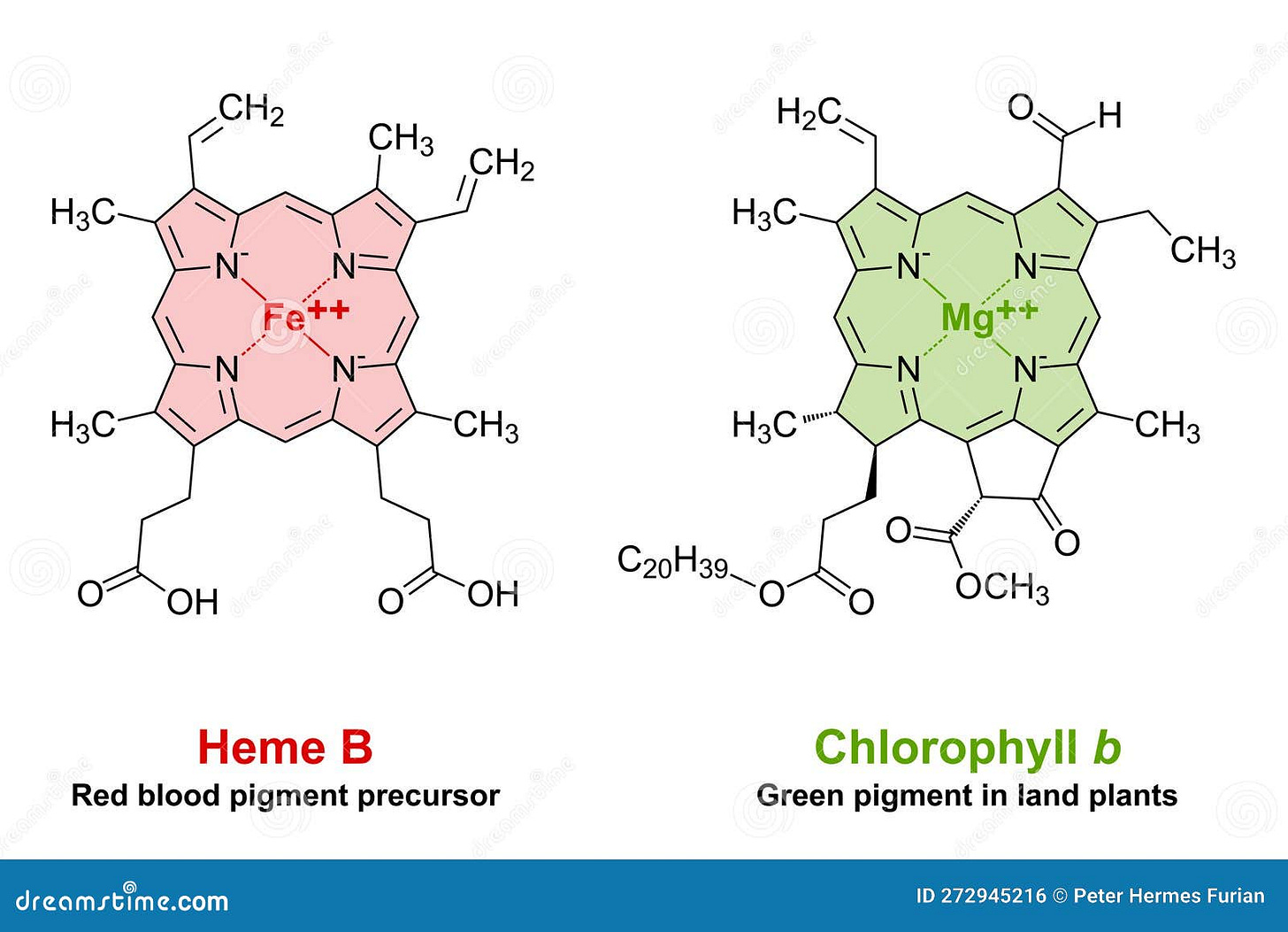
Hemoglobin is a globular structure composed of 4 protein chains. Each chain has at its core a heme (B) group, which is a porphyrin. At the center of heme, iron binds oxygen. What is a porphyrin? Good question.
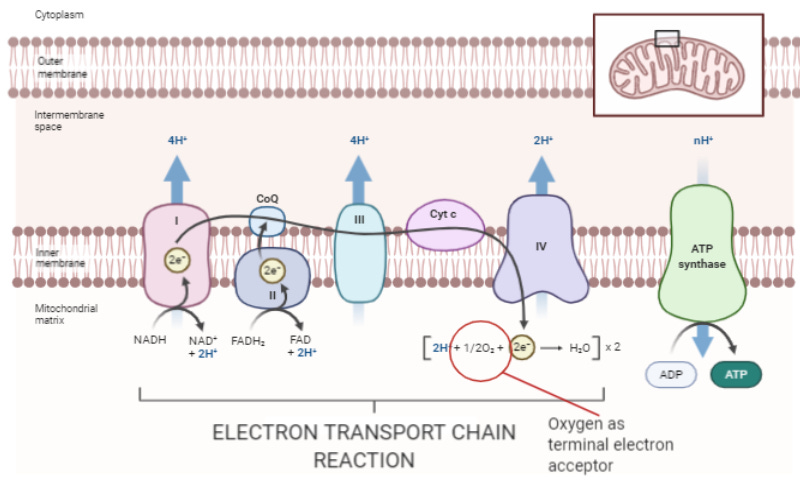
Porphyrins are complex cyclic organic compounds which absorb light energy, and make it available to the body for whatever reaction it needs to carry-on. This includes the creation of energetically dense molecules (aka photosynthesis), electron transfer to generate energy (cellular respiration via mitochondrial electron transport), and other chemical reactions.
In our mitochondria, the cytochrome c oxidase protein of the electron transport chain is composed of heme A. The heme in our RBCs (heme B) is not that different than the chlorophyll inside plants. Plants harness light to make food. Not so crazy to think that we do the same, now is it? Especially once you start to see how our blood vessels respond to sources of light (especially near infra-red light).
The rest of blood is a combination of fuel & white blood cells. Fuel consists of nutrients, energy-dense macromolecules, lipid particles, etc. I’m using ‘fuel’ broadly here.
But, between the water (which also responds to near infra-red light) and hemoglobin…the vast majority of blood is a medium that harnesses, stores, and transmits light & electrons.
“What about the oxygen?!”
Oxygen is the terminal electron acceptor of the electron transport chain. Its role is to create an outlet for the electron flow (i.e. current) used to make ATP (energy). Nutrients & light give us the excited electrons which go on this journey that ultimately lead to oxygen.
Beautiful, isn’t it?
How Does Blood Flow?
I wouldn’t blame you if you thought that blood flow was solely determined by contractions of the heart. However, recent experiments have proven that there is more to blood flow than the heart.
Even our understanding of the heart itself has recently come under scrutiny.
For centuries, we have believed that the heart is an organ composed of 4-chambers which synchronously allow flow of blood into its chambers, and actively contract to expel blood out of the heart.
This framework is rooted in the work of William Harvey - a physician of the 16th century.
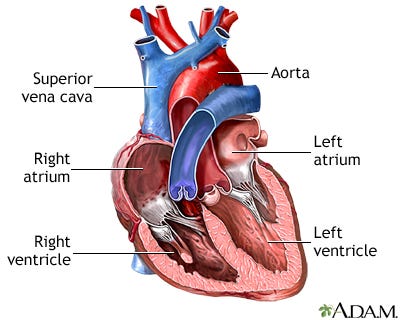
More recent anatomic discoveries by Dr. Francisco Torrent-Guasp (Paco) paint a different picture. Paco has pioneered a model known as the ventricular myocardial band. In this model, the atria are merely distended chambers of the circulatory system, and the functional heart includes the pulmonary artery, right ventricle, left ventricle, and aorta.

This new model of the heart, which demonstrates one long muscle twisted upon itself like a rope, is in agreement with the observed mechanical and electrophysiologic activity of the heart. Both electrical activity and muscle contractions proceed along the length of this muscle to ultimately result in ejection of blood through the aorta. In this sense, the heart undergoes peristalsis - just like the gastrointestinal tract.
Not only has Paco pioneered a new anatomic understanding, but based on this model a new surgery has been developed for those with congestive heart failure, eponymously named a pacopexy.
In this model, the heart isn’t an organ that lets blood flow in and pushes it out. In reality, the basal loop (piston chamber) wraps around the apex (piston). As blood moves from the basal loop to the apex, the apex finally contracts and ejects blood through the aorta whilst simultaneously moving the basal loop back up - creating a sucking force. The heart, indeed, sucks blood in from the vena cava. As observed by Galen himself.
“The overlying heart, at each diastole, robs the vena cava by violence of considerable quantity of blood.”
-Galen
This sucking force leads to a tapering chamber (a cone in 3D) which creates a vortex of blood flow, which imbues the moving blood with forward momentum that is finally aided by the contraction of the apex.
This is how the heart “pumps.”
…and the blood vessels?
Several animal experiments have demonstrated that after an animal is euthanized…blood continues to flow.
You may think this is trivial, and its probably because of some tension/pressure that remains within the circulatory system from a recently beating heart. Others suggest its due to contractions of the vasculature itself.
Pollack et al decided to test these “explanations.” In their most recent paper (October 2023), they use a chick embryo model to demonstrate the movement of blood hours after the embryo had been euthanized.
Particularly interesting is the substantial increase in flow-velocity while exposing the blood vessels to infra-red light.
Why?
Pollack et al have previously demonstrated the ability of infra-red to promote the formation of an exclusion-zone water boundary along the inner wall of the artery, which in combination with the electrostatic charge around RBCs generates a surface-induced flow. If you are not yet familiar with Pollack’s mind-blowing work on water and its role in biological matter, I would highly recommend it
In essence, the electrostatic interaction between negatively charged RBCs and the negatively charged water boundary along the inner lining of the artery results in a forward motion of blood. Infra-red light broadens this charged water boundary - thereby promoting forward flow.
And it does so in the absence of a beating heart.
Why Does Blood Flow?
To answer this question we borrow concepts from the first question above.
Blood provides nutrients, minerals, oxygen, and energy captured from light to all of our organs.
Every organ regulates the movement of blood flow to itself (and some regulate the movement of blood to other organs by hormonal secretions). Typically, organs which are in use increase flow to themselves.
A brain which is actively computing high volume of neurochemical signals increases blood flow to itself.
After you eat, the gastrointestinal tract which is digesting and absorbing nutrients increases blood flow to itself.
If your heart needs to beat more forcefully or with higher frequency, the coronary arteries will dilate to provide more blood circulation to the heart muscles.
Conversely, organs which are not used do not have a need for blood supply. The sedentary organ combined with the chronically low blood supply may result in the atrophy of the organ. The best example of this is with muscle. If you don’t use your muscles, they get smaller and smaller…and the limit to which you can generate force with them continues to decline.
Another example is with bone. The slogan “use it or lose it” comes to mind when learning about bone physiology in medical school. To some extent, this is true. If you do not put the bone under weight or stress, then it has no reason to fortify itself. Eventually becoming weak and brittle.
Finally, we have the case of cell death. As cells of an organ die, the amount of blood it needs to perfuse this organ decreases. Both atrophy and death result in diminished blood supply to an organ.
This makes perfect sense. We see this in chronically diseased organs, including the brain.
But, this has an often overlooked consequence. In fact, I have yet to see anyone point out this quirk of fluid dynamics.
Blood supply starts at the aorta, and continues to divide into innumerable parallel paths of flow. Thus, circulation is a parallel circuit.
Parallel circuits (as opposed to circuits in series) have unique properties both in electricity and fluid dynamics. One of these is related to its resistance.
In the above example, the total resistance of the circuit is a function of the individual resistance of the smaller vessels. R = 2.86.
What happens if one of these vessels dies or atrophies as a result of disuse?
If we stop using R3 (20), then R = 3.33. Resistance goes up!
If we stop using R1 (5) instead, then R = 6.67!
Do you see?
As more vessels in this parallel circuit die…resistance goes up.
What happens when resistance goes? Blood pressure must go up!
Thus, whether you are chronically ill or chronically sedentary…you create conditions which result in a net increase of resistance across your circulatory system.
Ultimately, leading to hypertension.
Part 2
Understanding Blood Flow & Pressure | Part 2
Moving On… In Part 1 we covered a foundational set of ideas about the nature of blood and circulation, including: What blood is. How blood flows. Why blood flows. If you ha…









Interesantes y poco conocidos planteamientos que involucran la química y la física así como nuevos planteamientos de la anatomía cardiaca en el fenómeno circulatorio de la sangre así como las causas de su atrofia. Muy útil artículo.
So this is the reason in recent comparisons that near infared saunas give the most benefit?