The Treatment Makes the Disease
Doctors will often try to do something instead of nothing. It makes them feel better. But, what about the patient?

Background
I recently wrote an article talking about a topic that has fallen out of the modern medical lexicon. The topic was cures.
Strange, isn’t it? You would think that cures would be one of the most commonly used words in healthcare. Unfortunately, it’s used less frequently with each passing year.
Instead, doctors talk about “managing” disease.
Cures are so primitive. In the modern age, we strive to manage.
In the above article, I made the case that cures come with side-benefits and that “treatments” come with side-effects.
To build on that idea, I am going to make an even more contentious claim.
In many cases of modern medical practice, the treatment is the disease.
Or, the treatment makes the disease worse.
Let’s start with a brief example to illustrate the problem. Then, we can move unto yet another story of medical mismanagement involving a loved one.
Diabetes
Diabetes is one of the most common chronic medical conditions plaguing the developed world. With the expanded use of artificial lighting and electromagnetic frequencies, it is now also plaguing the developing world. Thin diabetics are now in vogue.
But, what is diabetes?
Most doctors agree that Diabetes Mellitus Type 2 (the most common acquired form) is characterized by insulin resistance.
As the term suggests, this is a pathologic state in which cells that normally respond to insulin in an effort to extract sugar from the bloodstream…are no longer responding appropriately.
That is to say, in the diabetic more insulin is required to effect the same response. Why this is the case, is beyond the point.
Being in this state of resistance is bad for many reasons. First, and most obvious, is a reduced capacity to deal with loads of sugar in the bloodstream. This sugar can cause problems with many proteins and cells as a result.
Another problem that is not often discussed about is the consistently high level of insulin release. Why?
Insulin is a growth factor.
Growth factors do many things, including favoring storage of energy and macromolecules. This makes you fatter.
Another thing growth factors do is stimulate cells to grow. This increases the risk of developing cancer.
This is why diabetics have increased lifetime risk of various cancers.
Naturally, the cure to this problem is to improve insulin sensitivity.
But, that’s not what modern medicine does.
Instead, modern medicine gives people more insulin.
This makes them more resistant, and naturally requires patients to take higher doses over their lifetime to “maintain” their blood sugar.
This cycle leads to increasing doses of a drug that causes obesity and cancer, whilst simultaneously worsening insulin resistance.
The treatment, in this case, is the disease.
At the very least, it is indistinguishable from the disease.
Story Time
Let’s shift gears to another disease.
Recently, we returned from a trip to visit my in-laws. One of the purposes of this trip was to check on my wife’s grandfather, who has been treated for Parkinson’s Disease for the last several years.
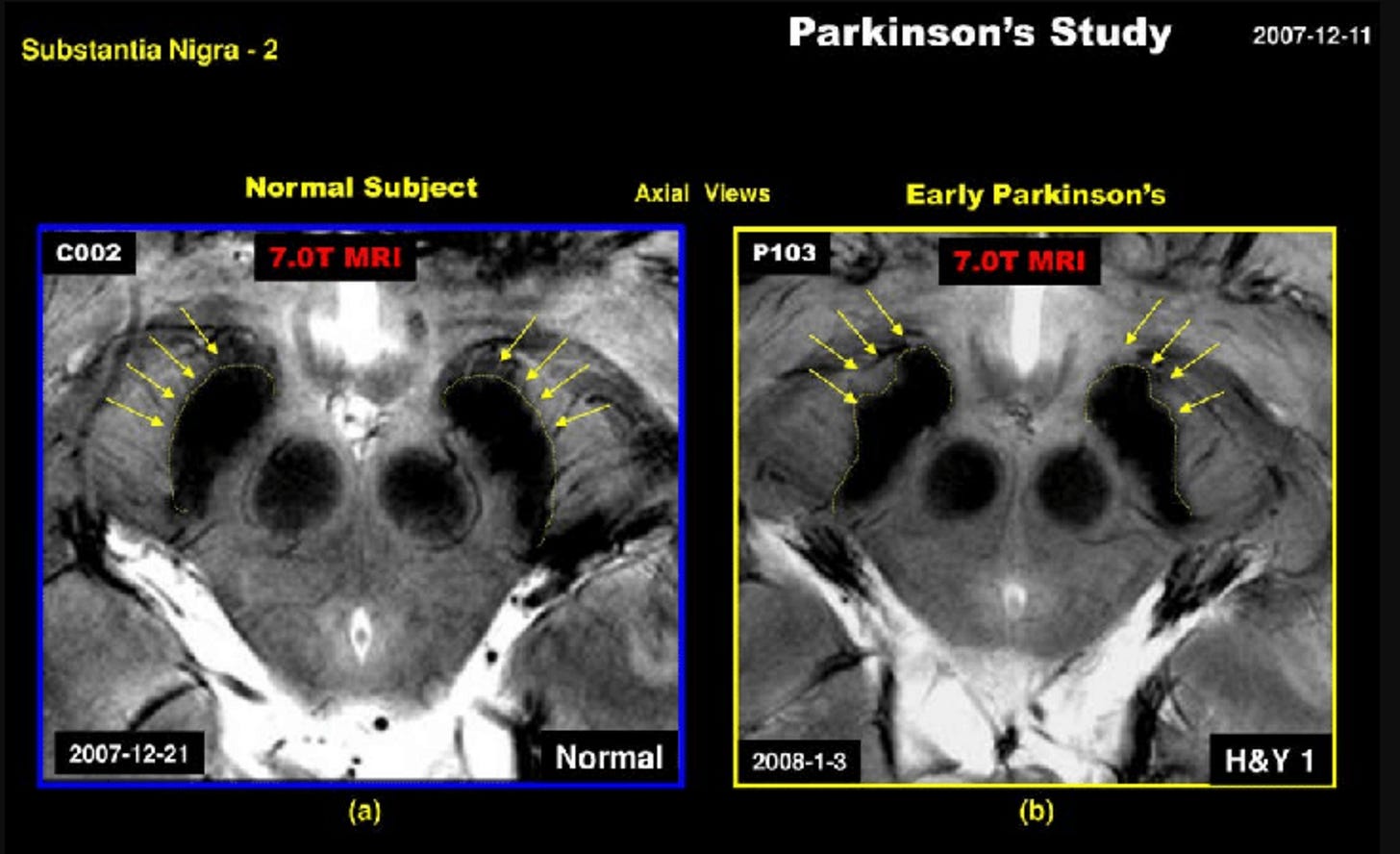
Briefly, Parkinson’s Disease is a degenerative neurological disease characterized by abnormal movement and inability to maintain fine motor control. It is believed that this is caused by the death (or reduced function) of dopamine-producing neurons in a region of the brainstem called the substantia nigra - or black substance. It bares this name because it is here that melanin is produced in large quantities, which gives this area its dark appearance.
Under this framework for the disease, it is then proposed that increasing the presence and activity of dopamine in the body is a sufficient standard for “treatment” of Parkinson’s.
This is precisely why the standard treatment for Parkinson’s is a combination of L-DOPA (levodopa) with other substances that prevent the degradation/recycling of dopamine, generally increase the activity of catecholamines (e.g. dopamine, epinephrine, norepinephrine), or increase the stimulation of dopamine receptors.
This treatment is exactly what my wife’s grandfather has been receiving in a futile attempt to curb his Parkinsonism.
There are many problems to discuss here including:
What really causes Parkinson’s?
What is an appropriate treatment approach?
But, before we get to those…we should give the devil its due.
Let’s assume that the above framework for diagnosis and treatment are valid.
Does this paradigm work, and what are the consequences?
Does the treatment make the disease worse?
Years of “Treatment”
To understand this story, we need to know why grandpa was being treated in the first place.
Several years ago it was observed that grandpa had trouble turning corners. It wasn’t that he couldn’t turn a corner, but that he had to shuffle around them. Otherwise, he could walk. Maybe not as fluidly or briskly as a young man, but at this point grandpa was 80 years old.
For the sake of argument, let’s say he had some motor deficiencies that plausibly suggest a Parkinsonian degenerative process. But, in terms of functional limitations, there was very little.
The first medication he was prescribed was a dopamine-promoting patch. Transdermal (skin absorption) infusion of this drug over the course of 24 hours.
His ability to walk did not improve, and he developed some side-effects. He really did not like this patch, and often removed it himself whilst family wasn’t aware.
This went on for some time, with no improvement in sight.
Then, the doctors decided to add a combination drug (with L-DOPA). Ultimately, he was instructed to take this pill four times per day. This was in addition to the patch.
One of the side-effects he developed was insomnia. For this, he was prescribed an anti-depressant and melatonin.
His original movement problems? No improvement.
But now, he also had difficulty sleeping. As one would expect, this would exacerbate any neurological problems, including motor coordination.
Present Circumstance
During my trip, I had many days to observe Grandpa’s disposition.
What I saw was depressing.
A man in his 9th decade of life who appeared to be drugged out, no improvement in his motor function, and with a laundry list of new problems.
For starters, he cannot sleep at night. He either lies awake in bed, or tries to get out on his own (since everyone’s asleep) and eventually falls in the dark of night. Did I mention his original motor problems have only gotten worse since being put on medications?
Second, he has a ravenous appetite. I have never seen someone eat so much in his age, and lose weight. People one third his age cannot eat this much without gaining weight. In my estimation, this is a consequence of rampant catecholaminergic (adrenaline) activity from the medication. His appetite and metabolism are ramped up.
Finally, and probably most bittersweet…he is completely lucid. Apart from the fact that he cannot get a night’s rest, and mumbles quite a bit…he doesn’t seem to have cognitive impediment of significance.
He still reads his newspapers and does the crossword puzzles. Point to any plant outside, and he will tell you its formal scientific name. Ask him which turn to take in town, and he will tell you.
Treatment Is the Disease
Before we get into what I believe Parkinson’s is, and how we can go about improving the lives of those who suffer from it…let’s address the elephant in the room.
With this treatment paradigm, we have a problem similar to insulin resistance.
If indeed Parkinson’s is a direct result of low-dopamine activity in the brain…then artificially giving a person dopamine will not help. Why?
Well, for starters…anything you give a person that they can produce themselves will have an inhibitory effect.
For example, if I normally make dopamine…but then you give me exogenous dopamine…then my body will turn down the pathway it uses to make dopamine endogenously. The body is smart. It knows that it has enough dopamine, and doesn’t make any extra.
So, if I have low-dopamine producing capacity…giving me exogenous dopamine will only reduce the already low activity of my dopamine producing cells.
This can manifest in a couple of problems. For example, if you’ve been taking medication for a while…and you start to notice worsening motor problems just before your next dose, your doctor may think that it’s “just your Parkinson’s getting worse.”
But in reality, the medication is exacerbating the alleged problem (low dopamine production). In response, the doctor then increases the dose of the drug that making things worse in the first place. This results in a spiral.
Eventually, Parkinson’s patients stop responding to these drugs the same way that they did before, and have to look for increasingly more desperate solutions. Such as deep-brain stimulation.
It Gets Worse
If indeed the problem is low-dopamine to begin with…then why do people get more (and sometimes worse) motor problems from the treatment?
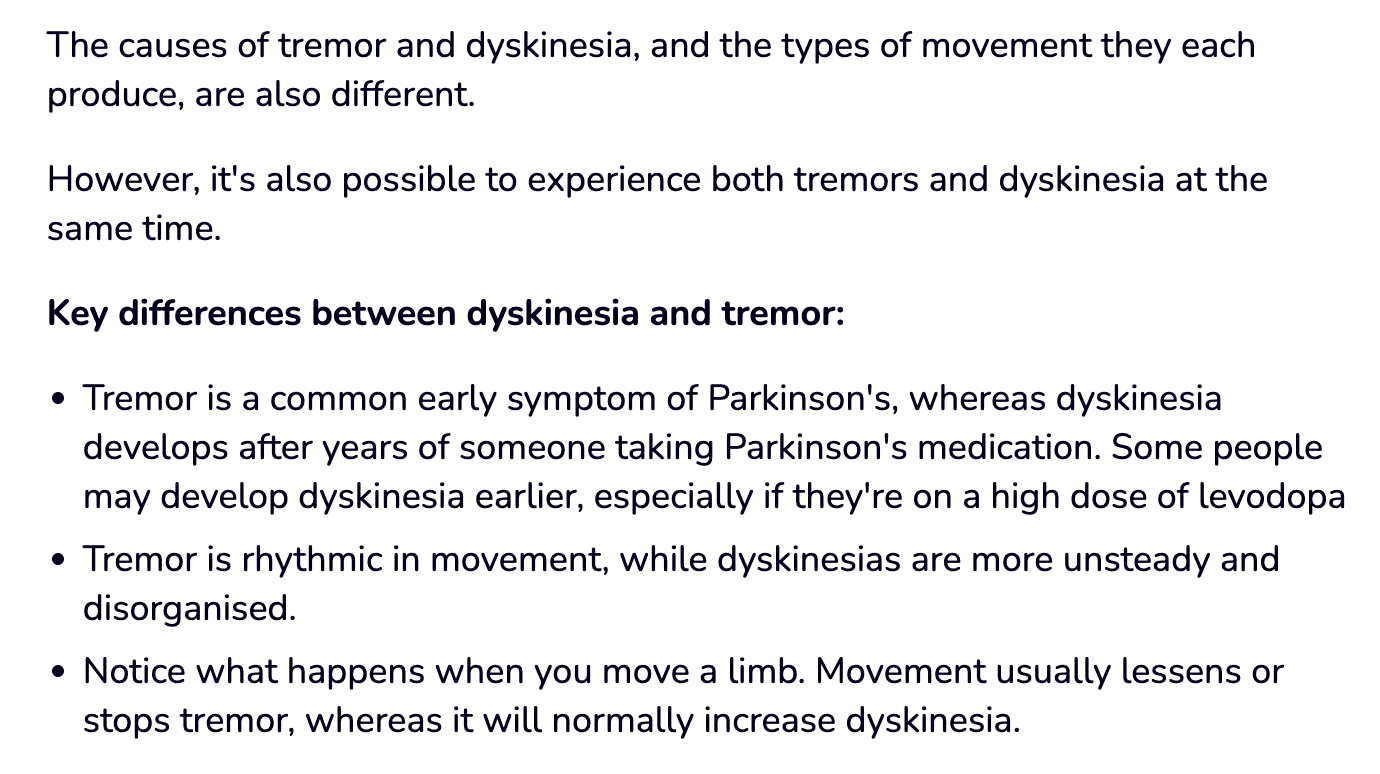
Motor problems like involuntary movements called dyskinesia. The official Parkinson’s literature goes to great effort to explain to patients that dyskinesia is different from tremors (shaking common in Parkinson’s)…so don’t you go thinking that the treatment is causing the same problems it claims to improve. It’s causing more motor problems, but it’s a different sort of motor problem.
At the end of the day, you came into this treatment with a motor problem limiting your life, and you’ve developed another motor problem limiting your life.
A New Perspective
To give credit where it is due, it was Jack Kruse who led me down a new path of investigation with regard to Parkinsonian syndromes.
Everything we have discussed so far has been based on the assumption that Parkinson’s is strictly a disease of low-dopamine production. There’s more to this story.
First of all, loss of the melanin in the substantia nigra is a hallmark of Parkinson’s.
What is less often discussed is that there is another part of the brainstem called the locus coeruleus that is also lost. This part produces norepinephrine, and is referred to as the blue spot, also because of its melanin content.
From this finding alone, we need to start considering a more unifying culprit in the development of this disease.
When you add to the observation that simply replacing the “lost” dopamine doesn’t fix the problem…the need for a better explanation becomes stronger.
What is melanin, anyway?
Melanin is a pigment. Some argue that it is the “darkest” pigment there is - that is to say, it absorbs all frequencies.
In addition to absorbing EM frequencies, melanin is also involved in the binding and clearance of many toxins in our bodies, including metals.
This may be related to another interesting finding in Parkinson’s, which is the presence of metals in the brain of the diseased.
What if high metal exposure depletes melanin, because it is being used to bind and neutralize the metal?
So, how is melanin made?
The image above shows us the path of converting the amino acid Phenylalanine into Dopamine, Norepinephrine and Epinephrine. As you can see, L-DOPA is an intermediary.
Here we see the series of reactions that produces indole quinones from epinephrine and norepinephrine - AKA adrenaline and noradrenaline in the previous figure.
Melanin (of which there are various types) is a polymer of indole quinones.
Why does this matter?
For starters, melanin is a conductor of electrical signal. That is one of its primary functions. It absorbs light energy and moves electrons.
Jack Kruse believes that it is the presence of melanin which allows catecholamines like dopamine to have predictable and functional effects. In the absence of melanin, both dopamine and melatonin signaling become chaotic.
The chaotic nature translates into chaotic movements and impulses - as we see in people with Parkinson’s.
The implications of this are quite profound.
For starters, if your melanin is degraded…then no matter how much dopamine you give someone, you cannot fix the problem. Because, apart from the fact that melanin is made from dopamine…the enzymes involved in its production require additional signals to make melanin (signals like UV-A light).
Secondly, if you are in an environment which promotes the degradation of melanin…then you will experience the sort of motor and impulse chaos that characterizes Parkinsonism.
Why? If melanin is a polymer of dopamine/norepinephrine…then breaking this polymer down releases more dopamine and more norepinephrine.
Even if by flooding the body with dopamine, you can slightly shift the equilibrium towards production of melanin…unless you address the underlying obstacles to melanin production, this benefit will be short-lived and ultimately result in worse symptoms.
Also known as “your Parkinson’s is getting worse” OR “it’s dyskinesia caused by the drug.”
Another In-Law
After long conversation, I was finally able to convey these ideas to Grandma and other family members. Ultimately, my impression was that Grandpa was being mis-managed, and that alternative approaches need to be considered.
Of course, this was met with some skepticism.
Coincidentally, another member of my wife’s extended family also had Parkinson’s. He’s had it for longer than grandpa. So, we paid him a visit.
To our surprise, this man appeared much more functional. He could walk on his own. Talks with clarity (although he is soft-spoken by nature). Has control over his appetite. Sleeps well. Appears well put-together.
What was he doing differently? The in-laws were very curious.
For starters: no transdermal dopamine patch. He regularly saw a homeopath and acupuncturist who would treat his complaints as he experienced them. He only took one levodopa combination pill, split into halves.
The difference in treatment approach and outcome was stark.
So stark, in fact, the family had no choice but to contend with the fact that I was onto something. More importantly, they had come to see that what his doctors were doing was wrong.
The Right Approach?
I don’t want to get too whimsical here, as I’ve never been formally involved in the treatment of Parkinson’s.
But, I will leave you with this much.
If the reality is as we suspect, and melanin is the core culprit…then the baseline treatment approach should start with rebuilding melanin.
How this is done is somewhat complex, and may be the topic of another article.
But, here’s what we need to consider:
UV-A and Infrared light
DHA, preferably from seafood
Stop habits which degrade melanin
Exposure to artificial blue light and non-natural EMF
Certain elements of our diet which inhibit melanin production






Dear Remnant MD, I firstly want to thank you for the time and energy you take writing about all these topics. Although I don't always understand everything (no medical studies), I worked for 3 years ( until very recently) on a neurological rehabilitation station in a clinic as administrative staff. Needless to say that the co/ro/na time was eye-opening for me and I used that time and my job to...research. Mostly elderly patients coming to us, after a stroke or/and some other neurological conditions+other colletaral diseases. Their med plans look almost copy-paste ...of course statins everywhere. After that, I found your thread and I just...never wanterd to write any comment ever..but everything you write about is on point. For the people ....it so heartbreaking. I saw what they eat, I see how the disease is being treated. No one gets off of meds. No one heals ever. They just get their symptoms managed and some are very happy when they go home walking and not in wheelchair or to a nursing home.
My mother in law has Parkinson for a long time. Never used mobile phone that much, she loved and loves the sun,no sunscreen, never smoked, never drank. She even had a heart attack a while ago and I guess it was a side effect from all those meds. I cannot help, I don't know how...I can't do anything. They all believe in these doctors like they are some Gods who keep the keys of the fountain of life and health ...and most of them just copy paste a medication plan and they try this year this new medication, then the other one, and the next one. They enroll patients in studies for pharma, take some blood for tests and ...that's it. Of course they tell you to drink more water. Very important, drink more water otherwise the brain schrinks.
Sorry for the rant, but this is what is like for regular people who see and are to some extent awake, to live in this world and have no real medical care if needed : it is heartbreaking.
Skin cancer would be another example of the “treatment” is the disease. Covering the largest organ of the body with chemicals every time you go outside then the doctor trying to assuage the worry by saying “good thing we caught it early” when he diagnoses your skin cancer. And that is not to mention the pervasive chemicals in soap, “body wash,” detergent, etc. I make my own soap and laundry detergent.
From what I’ve read here, I’m beginning to think melanin is at the root of almost everything.