Lowering Blood Pressure Without Prescription Drugs.
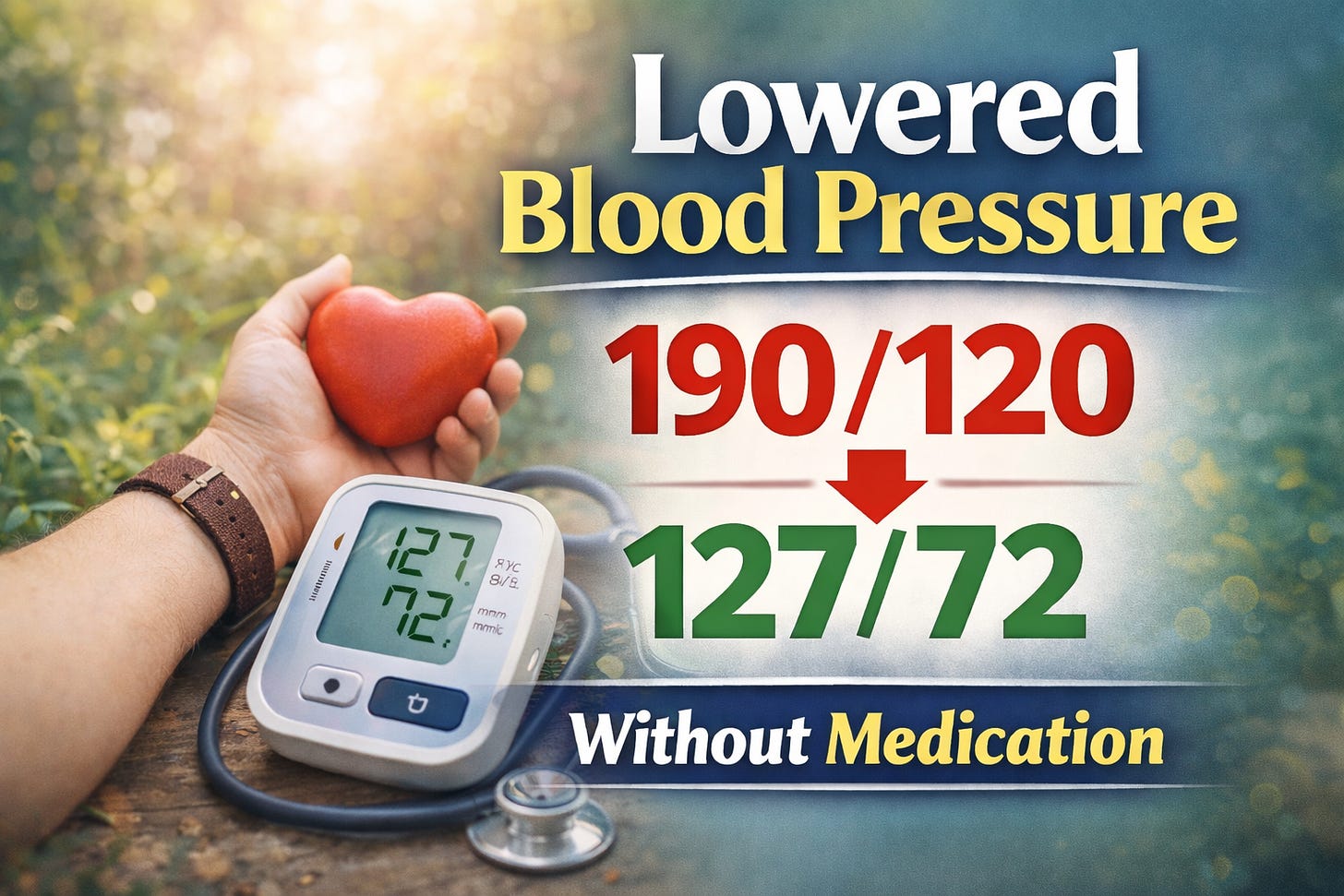
My mother came for the holidays with a blood pressure >190/120 mmHg. In 4 DAYS, we got it to 127/72. Here's how we did it.
Background
For as long as I have been in medicine, my mother has had trouble with her heart and blood pressure. In the past, she would mostly heed the advice of mainstream medical experts and rely on prescription drugs to manage it.
As a short-term strategy, this can be of benefit (I use that word loosely). However, it is nowhere near optimal as a long-term strategy for your cardiovascular health.
As it is for many people, short-term is often all they look for.
In more recent years, Mom’s been more amenable to my approach. She’s been reading this publication since the first article, and I think over the years has read your feedback, experiences, and learned enough from the articles to start taking holistic approaches more seriously.
In the last 6 months, my parents had a drastic change in their lives - in the best way possible. They are finally living the life they’ve always wanted. Unfortunately, this change in environment has also been accompanied by a drastic change in my Mom’s blood pressure.
When they arrived for the holidays, I measured her blood pressure (henceforth referred to as BP) and was shocked to find it was floating around 190/120 mmHg. In one reading, we saw a systolic of 197!!
In this article, I will discuss how we got her BP under control without the use of medications.
If you want to first learn my framework for understanding blood pressure, I would highly recommend checking out this 2 part series:
Furthermore, if you want to know why I disagree with the mainstream approach to measuring and treating blood pressure, read this article:
Now, lets dig in.
Dispelling some misunderstanding.
Some more astute readers among you would notice that the highest BP reading we got is ‘dangerously’ high. What’s referred to in medicine as “hypertensive urgency.”
Others have suggested that what I did was dangerous, and that I should have immediately taken my mother to the emergency room.
This demonstrates yet another misunderstanding of blood pressure and its management, which even mainstream medicine is slowly coming around to.
When I was in training, this is precisely the advice I would have been told to give a patient. Since hypertensive urgency used to be associated with a specific BP (> 180/110 mmHg), the standard suggestion would have been to seek medical attention and medically reduce it.
The more up-to-date thinking is something like this:
Hypertensive urgency is no longer used
the cutoff used in the past (180/110) is arbitrary
Now, we identify at-risk patients with “severely high blood pressure” and risk of organ damage
i.e. people with congestive heart failure or chronic kidney disease
As it stands, hypertensive emergency is a term used for those who have high blood pressure and evidence of acute organ failure.
Hypertensive urgency is can be used to identify people with “severely elevated BP” and risk of organ failure.
Any way you slice it, the recommendation for urgency is this:
Seek medical attention.
Slowly, reduce the blood pressure. Ideally over 12-24 hours.
Rapid reduction of blood pressure that high is risky.
As far as I am concerned, we satisfied both requirements.
I am medical attention.
And, we slowly reduced her blood pressure over days.
Diagnosing ‘High Blood Pressure’
First of all, I don’t believe in hypertension. Let me explain.
The idea that there is this disease called ‘hypertension’ is fallacious.
In fact, it is so fallacious that the medical industry has decided to give it a name: essential hypertension. Sounds very normal and expected, doesn’t it?
Well, you should know that essential hypertension is also known as idiopathic hypertension. Idiopathic is fancy for “we don’t know the cause.”
Which simply means that whoever diagnosed you with essential/idiopathic hypertension was not able to identify a cause.
Imagine walking around with a diagnosis that tells you more about your doctor’s ignorance than what is happening in your body.
If you come away from this article with only one idea, let it be this: blood pressure doesn’t go up without a cause.
You do NOT have hypertension. You do not HAVE high blood pressure.
Your blood pressure is elevated.
Just like you shouldn’t let a psychiatrist lead you to believe “you HAVE depression.”
You are depressed. Those are not the same thing.
Similarly, don’t let any doctor tell you “you HAVE hypertension.”
No. Your blood pressure is elevated.
The difference is that the former leads to “BP management,” whilst the latter leads to “WHY is my BP elevated?”
Now, we are asking the right question.
Finding the Cause.
Unfortunately, identifying a single cause for all cases of high blood pressure is a fool’s errand.
What I’ve tried to illustrate in the 2-part series linked above is that circulation and cardiovascular physiology is very complex. So complex, in fact, you are better off trying to understand how circulation works rather than memorizing a laundry list of possible causes.
Once you can get a rudimentary grasp around circulation, you can start to think about where your body is not having its needs met.
The circulatory system exists to provide energy, fuel, and nutrients to your body in one direction, and clear waste and depleted proteins in the other direction.
Every organ and body-part plays a role in altering the physical parameters of circulation which ultimately impact net blood pressure, which we measure in the arm.
Our lives and the decisions impact our organs, with consequences that determine the state of resistance and pressure that our circulatory system must adopt to account for the needs of the body.
What we ‘see’ as elevated blood pressure is the consequence of several preceding steps.
Any attempt to artificially reduce the number at the end of the causal chain (i.e. blood pressure) will not solve the problems which caused the high blood pressure in the first place.
Getting down to the basics…blood pressure is just a measurement.
Technically speaking, if you have ever had a doctor take your blood pressure the old fashioned way, the systolic BP is identified when he starts hearing a pulsing sound. This indicates that the pressure of the BP cuff has collapsed the artery (usually in the arm). Then, as the cuff is deflated the sound gets weaker and eventually vanishes altogether. At this pressure, we identify the diastolic pressure.
Thus, your BP is the systolic pressure at which the cuff causes your artery to collapse and the diastolic pressure at which laminar flow returns to the artery.
It is the job of a doctor to help you determine why the changes observed are happening. Not to simply put a label on you, and started prescribing a cocktail of blood pressure-related medications.
Treating High Blood Pressure.
As promised, we will now review step-by-step how we brought my mother’s BP down.