Why I Serve the Emergency Room as a Radiologist.
Many years ago, my life as a physician was going in one direction. Recent events derailed it towards a very different practice. One where I serve the emergency rooms of the US.
In recent weeks, there’s been a lot going on in our personal lives and I’ve felt the squeeze on all the things I’m trying to accomplish.
New baby
Home renovations and construction projects
Research and writing for Foundational Health
Hosting and tending to extended family
Serving my local hospital
I’d like to think I have these things handled, but one of the first signs that I’m spread too thin is when my body begins to pay the price. One of the benefits of caring for your health is that you also reset the homeostatic barometer which tells you when things are going wrong.
A sore joint. A headache. A runny nose.
All of these are signs. My body is telling me something.
It’s telling me I need to re-prioritize my time, at least for the moment. Which reminded me of another time I had to re-prioritize, but not for the moment…for the rest of my career.
Before the covid episode, I was on a career path that looked very different to today. One in which I would commit more of my time, resources and effort to the industry of academic medicine.
Mercifully, covid happened…and woke me up to the mistake I was about to make. The commitment I was about to embark on. A commitment to an industry that has little regard for both its practitioners and its ‘customers,’ so to speak - the patient.
That’s when I started this Substack. To focus my time, research and continued education on material that really moves the needle in people’s lives and their health. Material based on a framework that really understands the nature of being, and how and why disease manifests. Heck, even what disease is.
This shift in my focus had to be accompanied by a desire to move away from all the corrupt practices of my profession. To stop giving the institution more of my time. To be involved in cases I truly believed will help a patient.
People often say modern medicine is terrible when it comes to chronic disease, but excels at acute and surgical care. To some extent that is true, those are definitely where its strengths lie, if indeed these are traits unique to modern medicine. We won’t argue about that here.
But, this means that if I want to have a conscience while still working in this industry…then I had to shift my focus towards practices which do indeed have a positive impact in peoples lives. Or, at least with the potential to do so.
Enter the emergency department.
In a hospital, the ED isn’t only the ED. The acutely ill and trauma patients which come through the ED are also served by trauma surgeons and critical care specialists.
So, I figured…that’s who I will help. Those patients and those clinicians.
Now, granted…not every patient that walks into the ED and gets some imaging needs my help. There are a lot of wasteful practices, for sure. But, that’s beyond the point.
In the ED, the cases which have the potential for positive impact are far more frequent than in any other clinical setting.
Especially cases in which you can make a real difference in a person’s life, right now. I’m talking about the kind of cases where nobody else but the radiologist can know something of critical importance.
Let me explain what I mean.
This story is from the time that I was a trainee (resident) in a busy NYC hospital. I was on call…and the only radiologist in the hospital. An elderly lady came into the ED with vague abdominal pain. The doctor ordered a CT scan of their abdomen, and so I took a look.
I diagnosed an imminent closed loop obstruction.
What’s that? Glad you asked.
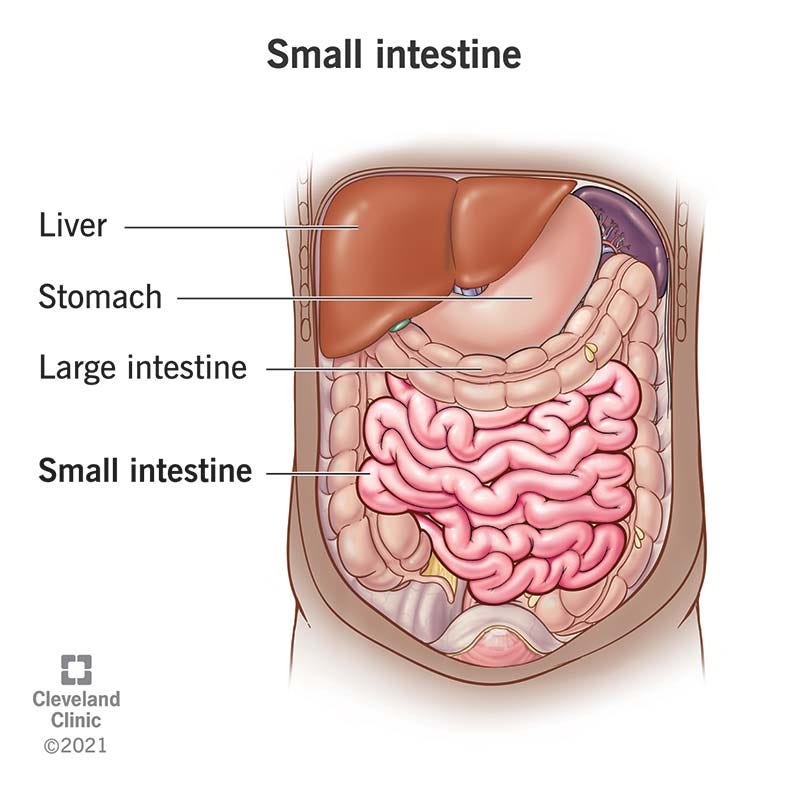
We have a very long small intestine (bowel) that is jumbled up onto itself in many loops.
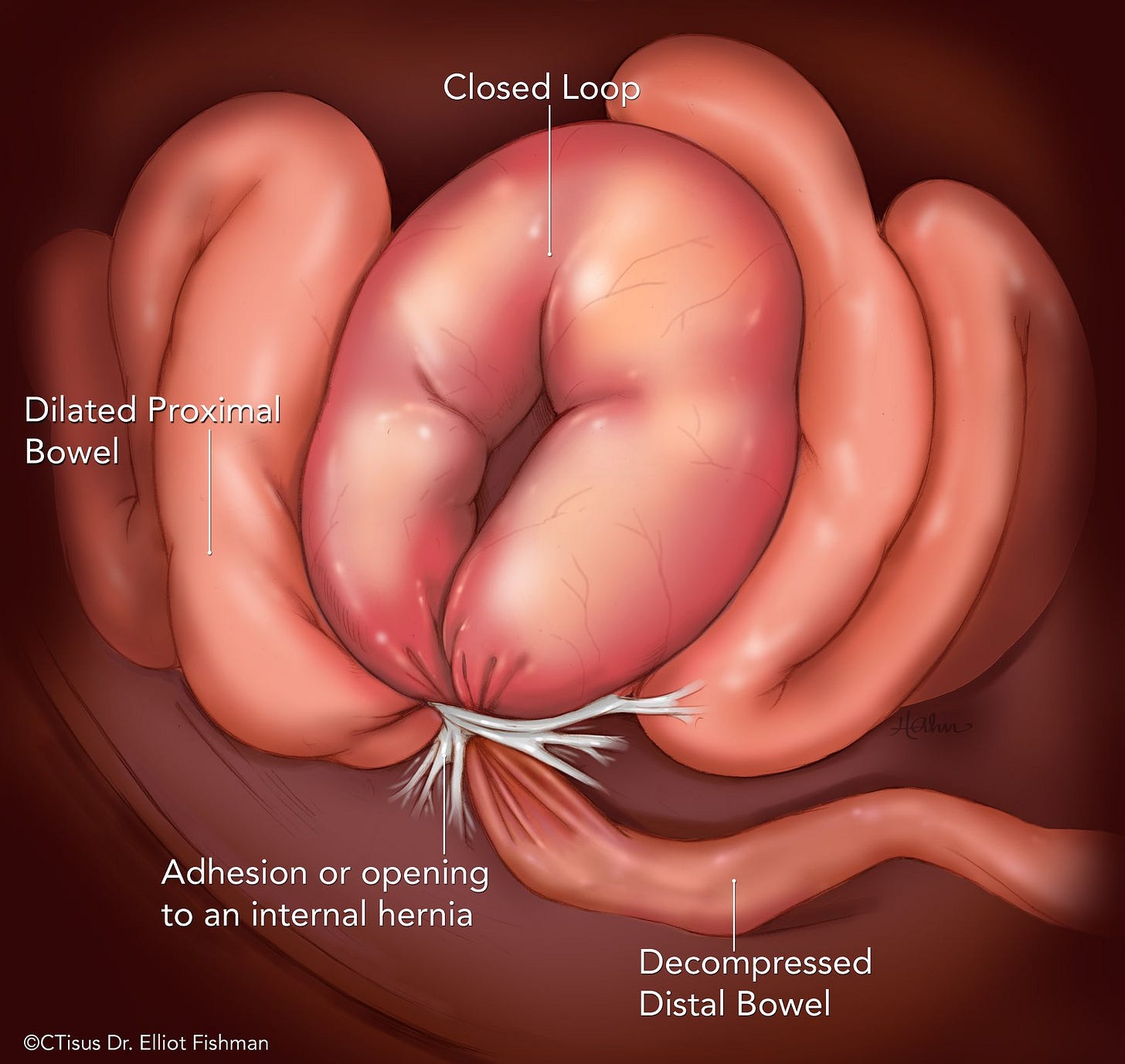
For a myriad of reasons, most commonly from scarring, one of these loops of small bowel can twist around a neck. This point can serve as a “bottleneck” which prevents the movement of blood into and out of that loop of bowel, putting it at risk of ischemia and infarction. AKA dead bowel.
Because of this twisted loop orientation, and compromised blood supply, the loop can start swelling…and the swelling just makes the strangulation and risk of bowel death even worse.
If left untreated, this can lead to dead bowel…which even in the young and healthy can be fatal.
As I like to tell my trainees, even a monkey can identify a closed loop obstruction/dead bowel after it’s already happened. The way that a radiologist can make a difference is to help clinicians identify these anatomic orientations which are at risk of becoming full-blown closed loop obstructions.
What I saw that night in that elderly woman’s abdomen was not a “textbook” presentation of a closed loop obstruction. What I saw were bowels that were oriented in such a fashion that the swelling and bowel death was imminent…though nothing had happened yet.
So…that’s what I told the team taking care of the patient.
Shortly after, the on-call surgeon walked into my reading room and disagreed with my diagnosis.
“Those findings aren’t convincing. The patient seems fine clinically. Just some vague abdominal pain.”
I walked him through the images and made my cases a little more thoroughly.
He still disagreed…and demanded that an attending (faculty physician) provide a second opinion. Unfortunately, I was only a trainee at the time…and the only radiologist present. But, I knew an attending at a neighboring hospital, and asked him to come by.
Once he arrived, I didn’t tell him anything. He just turned to the surgeon and asked why the patient was here. Then, he started looking at the images himself.
“That’s a closed loop,” he says to the surgeon.
looks at me
What did you tell them?”
“Closed loop,” I said.
Next evening I come in for my night shift, and immediately open up the medical records to see what happened to this patient.
I see a note from that night around 4AM, the patient started feeling a bit worse, and immediately the surgeon realized I was right, and took her to the operating room.
By his report, there was scar tissue everywhere in her abdomen. Which, as a side note…we can’t see on imaging. We can only see the consequences of this scarring.
He found the closed loop I was talking about, and fixed it. There was no dead bowel…surgeon had gotten their in time. Patient went home a few days later.
Although experiences like this are considered stressful and confrontational by many of my colleagues…it felt natural. More importantly, it set pieces in motion that I realized years later.
For those of you wondering what I do in my day-job…that is it. I help emergency teams identify and care for patients in dire circumstances. It’s fun, rewarding, and helps me sleep at night.
Even if our newborn doesn’t.
So, as much as I would like to spend all my time reading more ancient and medieval medical texts, writing, and experimenting with health protocols…I have a responsibility to some hospitals and their acutely ill.
As this digital business grows, one day I can do this full-time…and leave the modern medical industry entirely.
On that note, you may have noticed some changes to this website. I’ve received the final design package for the logo of Foundational Health. Hope you like the logo.
Things are slowly, but surely, moving in the right direction.



love this story
Doc, thank you for sharing this story and practicing medicine.