I'm Seeing Less Brain Aneurysms.
And, I'm not entirely sure why. But, here is my hypothesis.
Background
I am coming up on the anniversary of moving my family from the northeast (of North America) to the south. With this move came a new patient population, for whom I have the privilege of providing medical attention.
There were some changes that were expected, and some that were informative.
One that I’ve been paying attention to for the last several months are brain aneurysms, in part because I have always had a fascination with cerebrovascular disease and in part because I used to be afraid of brain aneurysms.
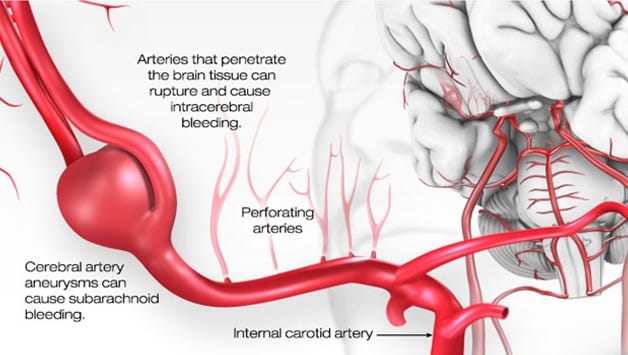
There are few things that can seemingly come out of nowhere and take the life of a young, and otherwise, healthy person. A large clot in an unfortunate location, or a ruptured brain aneurysm.
In fact, brain aneurysms are the most common cause of non-traumatic brain bleeds.
Once they rupture, the associated mortality is incredibly high. 25-30% are either dead or severely disabled before they make it to the hospital. That number rises to 50% within first 30 days of admission.
As a radiologist in the north, I would see “incidental” brain aneurysms a few times per day.
That is to say: As I would read a brain scan that was ordered for something else, I would incidentally find a brain aneurysm. Sometimes, I would find multiple in the same brain.
Since moving down south, I can count on my hands the number of incidental aneurysms I have found over the span of a year.
Stark difference in observed rates.
In this article, we will explore the nature of aneurysms, why they may form and rupture, and what can explain the observed differences in rates by latitude.
On Aneurysms
One of first topics with which I broke away from the centralized medical paradigm was in trying to reframe and understand the nature of blood vessels, how they remodel and when they go wrong.
The formation and rupture of aneurysms served as a good case study around which to build this new frame.
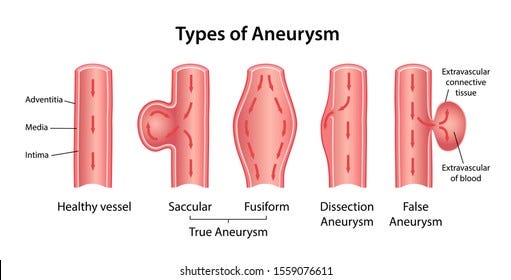
Aneurysms are focal expansions/dilations of blood vessels that occur in arteries of all sizes, from the Aorta to renal (kidney) arteries to small branch vessels inside the brain. Aneurysms come in all shapes and sizes.
Of the true aneurysms, saccular aneurysms tend to be the most common and most concerning.
The problem with these expansions is that the increase in surface area is accompanied with thinning of the vessel wall. Think of a balloon that keeps expanding until it finally pops.
The aneurysm, like the balloon, can rupture as the continued pressure from volatile blood flow causes the sac to increase in size beyond the capacity of the limited connective tissue (blood vessels are connective tissue) to fortify.
There’s a famous rule of “7” in the neurosurgical literature as it pertains to aneurysms in the brain. If the saccular aneurysm is greater than 7mm in size, there is far higher likelihood of that aneurysm rupturing and causing a brain bleed.
However, there is a problem with this threshold.
Because most aneurysms are small, a large proportion of aneurysmal brain bleeds are of aneurysms that are less than 7mm in size. Here, we face the conundrum that plagues the neurosurgical community.
Which aneurysms do you treat, and how do you know when to treat them?
As you can see from the image above, the options are many and varied. Option ‘a’ is the classic open surgical technique, in which a clip is used to exclude the aneurysm from the parent vessel. Option ‘b’ is a minimally invasive approach in which you navigate to the aneurysm using a catheter, and deploy a coil-mass to occlude the aneurysm.
Option ‘c’ is one of the more recent technologic advancements called a flow-diverting stent. The mesh of the stent wall is organized in such a way that flow to a dead-end is minimized, while flow to true vessels is maintained. This allows the aneurysm to slowly clot and close off over time (usually on the scale of days to weeks), while the parent vessel and any of its branches that may be covered by the stent continue to receive blood flow.
Truly a brilliant invention.
Risk Factors
As mentioned above, one of the difficulties in managing people with known aneurysms is to know when to intervene.
In the industry, the terms stable and unstable are used to refer to aneurysms which appear to be of high-risk for eventual rupture. This categorization is based on decades long observation of population data, most of which concerns ruptured vs unruptured aneurysms.
Less attention is paid to and less is known about the formation of aneurysms.
In my opinion, both formation and eventual rupture of aneurysms share many (if not all) risk factors and thus exist on the same spectrum.
One of the most robust risk factors for aneurysm rupture is cigarette smoking. Not entirely surprising as it is a combination of stressors on the body and blood vessel.
Other factors that are commonly discussed are high blood pressure, vitamin D, hormonal dysregulation (whether natural or iatrogenic), connective tissue disorders (not surprising), and in some cases ethnicity.
Differences Down South
Back to the difference I’ve observed in the frequency of aneurysms amongst my specific southern population.
And, I do mean specific. I have a feeling these observations do not generalize to any souther population. I’ll tell you why.
But first, let’s address why the observed rate are different - if indeed it is a reliable observation.
There are a few things worth knowing:
Many neurological diseases and inflammatory conditions seem to correlate with Vitamin D levels.
Meaning, the higher a person’s vitamin D levels (I believe by endogenous production), the less likely they are to have these conditions, the lower the severity, and the higher likelihood of recovery.
Nitric Oxide (NO) is a gas that plays an important role in the overall health and functional capacity of our blood vessels.
This is in part due to the variable interaction of NO and O2 (oxygen gas) within the mitochondria.
With that said, it’s worth noting some observations in the research:
There are seasonal and latitudinal variations in rates of aneurysm rupture
worse in the winter, worse above/below certain latitudes
I think you can start to see the picture I’m trying to paint.
Remember: it’s very likely that the constellation of factors which lead aneurysms to rupture, also lead them to form in the first place.
Southern states have approximately 2x the total hours of annual sunlight compared to northern states.
With this increased sun exposure, we can expect proportionate improvements in inflammatory stress including:
UV activated production of Vitamin D
Production of melanin & melatonin
Infrared activated production of NO
Infrared activated movement of NO from mitochondria to bloodstream
Improved electron configuration and availability of O2 for cellular metabolism
These are just a few.
That is all to say, through a compounded anti-inflammation, pro-repair and improved homeostasis effect…the blood vessels may be more robust and less likely to develop aneurysms in locations of increased vascular and mechanical susceptibility.
However, there are caveats.
For example, the local population should also have:
Tendency for outdoor activity to maximize sun exposure
Low cigarette & vape smoking habits
Low alcohol consumption
Otherwise, the strength of the observed effects may be blunted.
After all, you cannot appreciate the benefits of the sun if you stay indoors.
There’s also an additional effect, in that…the more time you spend outdoors the less you are exposed to artificial lightning, which can be pro-inflammatory.
That’s all to say, I believe the exposure to sun and nature are accounting for the observed differences.
I will keep an eye on this and discuss with my colleagues in other parts of the continent.
Hope you found this informative, and if you are interested in circulatory health and mechanics, check out the article on circulation and blood pressure:




Didn’t know that artificial light was pro inflammatory. It makes sense though. Being indoors under artificial light, especially fluorescent, lights feels increasingly stressful. Upon going outside into the sunshine, the feeling of relaxation and improved focus is almost immediate.
A very interesting read, thanks.
My spouse survived a ruptured brain aneurysm at 39, with no surgical intervention due to delays in diagnosis through broken down hospital equipment way back in 1990. On the final pre surgery prep scan, post head shave, it was shown to have healed, though there was still brain damage from the bleed.
Oh, and btw you are seeing fewer brain aneurysms, not less!