Coronary Artery Disease, Calcium Scores, and Surgery
Should we be operating on everyone with coronary artery disease?

Background
For many years I have been studying and contemplating the nature of vascular disease. The circulatory system has been a fascination since beginning this career.
It’s hard to explain why. For starters, the heart is so alive. Constantly beating - from birth til death. Without rest.
God forbid it take a break. If it did…we would start pounding the chest, injecting IV drugs or electrocuting it.
Then, you have the arteries and vessels. A road to every organ and body part. There are few modern aspects of medicine which are truly unique - one of these are minimally invasive intra-vascular surgeries. Professionally referred to as interventional radiology.
Despite this fascination, life ultimately led me to a different path. One in which I am always studying and diagnosing vascular disease, without intervention.
So, I will caveat the following analysis with this.
I am not a cardiologist nor a cardiothoracic surgeon. In some ways, this is a good thing. In others, it’s not. You be the judge.
Coronary Artery Disease
If you are an avid consumer of the digital health space, you will have noticed discussions about coronary artery disease, coronary calcium scores, and atherosclerosis.
This has become a particularly common point of discussion among both cardiologists for risk-stratification, and among low-carb/ketogenic/carnivore diet fanatics.
On the one hand, cardiologists pursue aggressive therapies for people with high calcium scores…and on the other, diet fanatics think they are healthy because their calcium score is low.
In my opinion, both of these views are misguided.
Why?
For starters, just because your arteries are mineralized (or calcified) does not mean they are obstructed. But, if they are mineralized and obstructed…it has a different significance.
Mineralization/calcification is a rather long-term process. Which means that if your arteries have slowly calcified and obstructed, but you haven’t noticed…the organ has collateral blood supply. This collateral supply can come from old vessels that have re-opened (usually congenital dormant tiny vessels). Or, the chronic state of oxygen-deprivation has signaled the proliferation of new vessels.
What this means is that the chronically obstructed vessels need not be re-opened. Because the organ already has another route by which it receives blood. This is typically called collateral supply.
On the flip side, just because your arteries have no calcification…does not mean they do not contain soft-plaque or undergone remodeling such that healthy laminar flow can be disrupted.
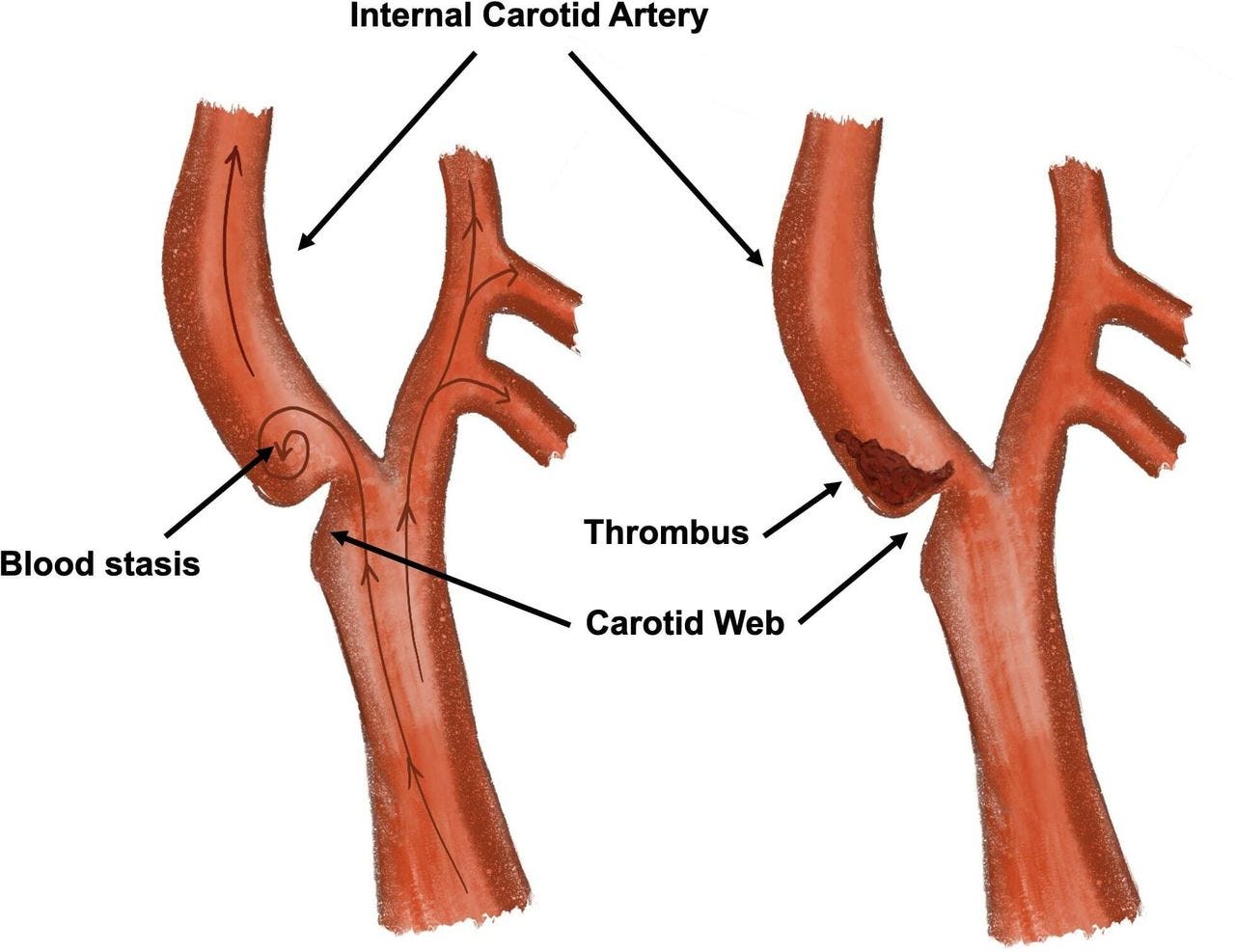
A good example of this are carotid webs.
Despite the fact that there is no atherosclerotic plaque at the location of the web, this ridge creates a zone of low-flow in which blood can become static and form clots. Which can then travel up the artery into the brain and cause a stroke.
As you can see, the problem of atherosclerosis and cardiovascular disease is not as cut-and-dry as most doctors and cardiologists make it out to seem.
Public Health Campaigns
If you live in a major north american city, you may have encountered public health campaigns.
These campaigns often take the form of promoting screening programs for various illnesses, such as cancer and heart disease.
What may seem like a well-intended attempt to improve public health, has less-than-benign practical consequences.
One of these consequences is that people who are otherwise asymptomatic or without clinical illness, will be lead down a path of testing and treatment which can result in harm they could have otherwise avoided.
Let me give you an example to illustrate what I mean.
Heart Disease & Calcium Scores
Take for example the recent rise in campaigns for being “heart healthy.”
Campaigns that are funded and organized by the very same organizations and institutions which have been “treating” heart disease for the last 50 years…all the while, the rates of heart disease and mortality continue to rise.
What does this program look like?
Well, you might find yourself in a community clinic in which someone promotes things like a lipid panel (to check your cholesterol) or a coronary calcium CT scan to check for atherosclerosis.
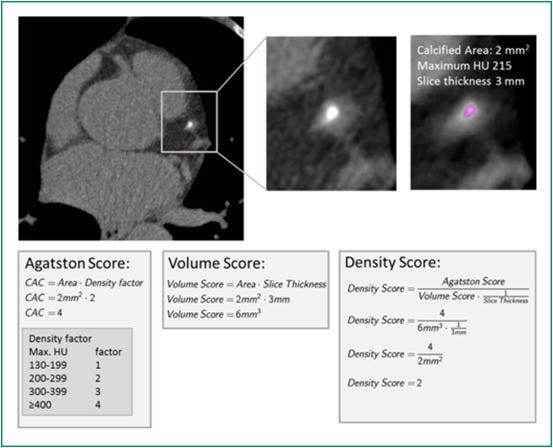
Coronary calcium seems to be all the rage today, both within the mainstream medical establishment as well as the alternative health space. Essentially, this is a test that gives an estimate of calcification burden along your coronary arteries. Based on the volume of calcification, you are given a risk score.
People tend to believe it gives them some indicator of their risk for future cardiovascular events (such as heart attack or stroke). To some extent, it does. However, this is not the only predictor of future cardiac risk…and taken as a factor on its own, it is of limited utility.
For example, let’s say you have a high calcium score. But, you have no other comorbidities such as diabetes, hypertension, prior cardiovascular events, and so on. You don’t even have any history of chest pain, or cardiac symptoms. No history of alcohol abuse or smoking cigarettes (which are huge risk factors). Just the calcium. What are you supposed to do with this high calcium score?
Should you undergo a surgery to revascularize the heart?
You see, almost all interventions have been initially designed and studied for secondary prevention - that is, to prevent a cardiovascular event from happening again.
In fact, the strongest case that can be made for statin use (if indeed there is ever a need to take a statin), is for secondary prevention.
But, what about surgery?
Should you, in the above example, undergo cardiac catheterization or open heart surgery?
This is where things get very messy.
Keep reading with a 7-day free trial
Subscribe to Foundational Health to keep reading this post and get 7 days of free access to the full post archives.