Case Study | 1. Hand Numbness & Spine Disease
My father had complained of numbness & tingling in his hands for years. Fiat medicine got him nowhere. One look at his spine, and the problem was clear. But, his doctors did not know it.

Background
For years my father had complained of intermittent numbness and tingling in his hands (and sometimes feet), usually in 1 or 2 specific locations.
From the perspective of modern medicine, he had many potential contributing factors.
Years of physical labor with repetitive motions
Chronic antibiotic use - specifically fluoroquinolones
At one point he was diagnosed with ‘pre-diabetes’ after he was put on a statin
Yes, statins can cause diabetes…
If these predisposing factors were not enough, a crack team of Neurologists has put together a diagnostic algorithm to figure out what is going on.
Simple, right?
Case Report
Maybe as his son, I have an unfair advantage in that I am very well aware of his history. The history of a presenting illness is probably the most important component of any patient-doctor encounter.
Unfortunately, taking a history is a dying art. Some say it’s physical examination skills - but, that art is already dead. Next on the chopping block is history-taking.
If you ask my father about his history of neurologic pain, he would recount the following:
Decades of migraines
Professional wrestling
Years of physical labor - including operating heavy machinery
‘cracking’ joints in his fingers, neck, and back for decades
Common things being common, this should prompt an evaluation of the nervous system. Which they did - after months and months of waiting. He underwent an MRI of his cervical and thoracic spine.
When ordered, this is usually the sequence of events:
Clinician orders MRI
Radiologist reads the MRI, and composes a report with this final Impression
Clinician reads the impression, without reading the body of the report or looking at the images
Clinician decides the problem is not related to the spine because of the wording in the impression
Let’s now take a look at my father’s MRI reports.
Cervical Spine MRI:
Thoracic Spine MRI:
The impression one gets from the cervical spine MRI is not concerning, though not technically false. If the ordering physician looks at that report, it is hard to fault them in thinking “his neck must be fine.”
Although the thoracic spine report is somewhat more elaborate, it will get dismissed because the hands are innervated by the brachial plexus, which is a convoluted mesh of the nerve roots from higher up in the spine:
So far, on the basis of these reports his doctor dismissed that this was related to a spinal nerve root problem.
After months of tinkering to no avail, he was referred to a neurologist who performed an electromyogram - using electrodes to gauge the activity of your peripheral nerves. This was also negative.
So, as far as his doctors were concerned - it was not a nerve problem.
Spine Lesson
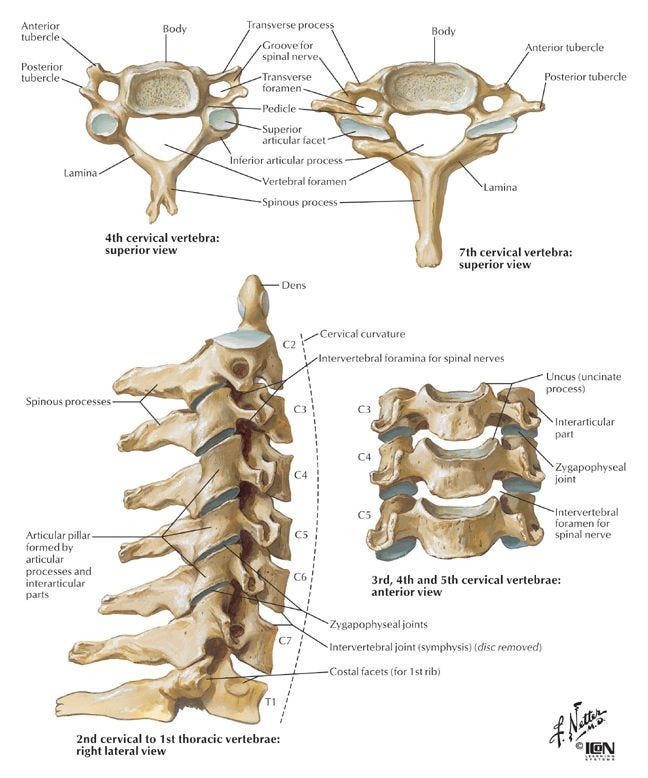
Before we look at my father’s imaging, let’s take a look at a normal cervical spine.
And an average (normal-ish) MRI of the cervical spine:
I don’t have the real estate to go over the spine in detail, but maybe a future video/presentation if the audience desires it.
When we look at a spine MRI, from a biomechanical perspective we look for a couple of things:
Degenerative joints including: articular facets, uncovertebral joints, intervertebral discs, ligaments
Bones
Neural foramen (from which nerve roots exit)
Spinal canal (which houses your spinal cord)
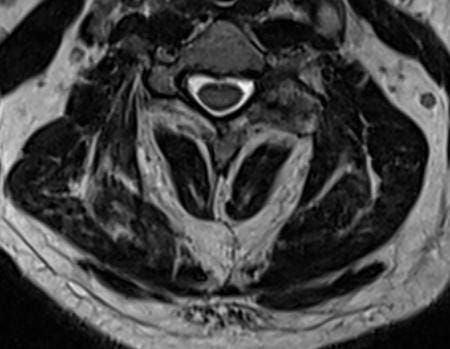
Now, my Father’s Cervical Spine:
Doesn’t look all that different, right?
Couple of things to note here…
First image:
Multiple levels of disc bulges and redundancy of the ligaments along the posterior aspect of the spinal canal - this narrows the available space for the spinal cord
Multiple levels of degenerative changes between the vertebral bodies & intervertebral discs
Second image:
Disease between the facets/joints as well as the discs & ligaments have resulted in narrowing of the neural foramen - causing compression of his lower cervical nerve roots.
Exactly at the level that supplies the brachial plexus - i.e. his hands!
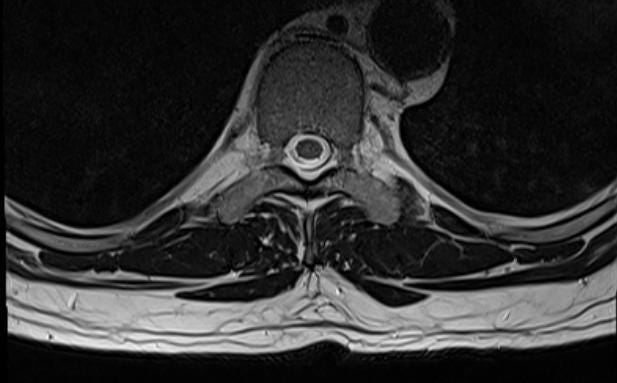
Now, his Thoracic Spine:
Again, what we see here are multiple levels of degenerative disc disease - although unusual for the thoracic spine, as it is a rather rigid component of the spine.
In his case, it is causing pronounced narrowing of his spinal canal, but also…the neural foramen…

At the top of this image you can see a black dot surrounded by white space - this black dot is the nerve root, and the white space is the surrounding fat. Normal, comfortable nerve root.
In the center of the image, you can see a black dot as well, but it is crowded by disc to the lower left, and ligament/facet disease to the lower right.
Taken together, these are all signs that the thoracic spine does not have as much support as it needs to maintain the downward weight and stress channeled through the spinal column.
Which brings us to the final and most commonly overlooked part of the spine…
What’s behind it!
If you take a second look through the images above, you will see that behind the spine is a lot of white. This white stuff is fat.
Look at these cross-sections…
Dark bands = muscle/ligmanet | White = fat
From my perspective, and taking his body as a whole - I can see that he doesn’t have robust muscles around his spinal column. Exceedingly common in the modern world because:
We sit at our desks…often hunched
We sit in our cars
We sit in front of the TV
We sit in meetings
When we go to the gym, we focus on what we can see - the front!
I concluded from his history and images that he has been neglecting the muscles of his back that support the weight and movements of the spine. Without this support, the spinal column can collapse on itself, and usually the first things to be impacted by this collapse are the discs.
With this collapse of the discs, you get impingement on the spine and the nerve roots.
My recommendation: work out your back muscles - focusing on intrinsic/deep musculature as well as the more superficial broad muscles.
Within months - his neuropathy resolved. No meds. No surgery. No unnecessary tests. No months of waiting to be seen by a consultant who doesn’t care.
What sort of back exercises? Just do something. I found him specific exercises & dedicated machines designed for back exercises. But, he did whatever he could with the equipment he had at home. A bench. A home gym machine. Barbells.
It’s now been more than a year…and his symptoms have not returned.
No surgery.
No medications.
Simple.











Late into my career as a registered nurse (now retired), I made the decision to leave hospital bedside 'sick care' to focus more on actual health care. After a few years of training, I became a massage therapist and quickly built up a clientele of oncology and orthopaedic patients.
I remember one lady, in her mid 40s, coming to me with complaints of arm pain/tingling. She had had rotator cuff surgery in the past and her doctor told her the pain/tingling was related to that. End of story except that during the massage, every time I tried to work on a particular part of her neck, I was able to elicit the arm pain/tingling. My advice to her was that although I wasn't a diagnostician, in her place I would get a second opinion with a surgeon who specialised in neck problems since that seemed to be the source of the problem. She did just that, and sure enough she had a protruding cervical disc.
I know doctors are pressed for time, but I despair at the lack of hands-on assessment these days. I lost count of the times in the hospital when a doctor was present and didn't even look at the patient, let alone lay hands on the patient. It does truly seem to be 'medicine by algorithm' now.
The first place you would look barring any red flags (history & basic examinations) would be the spine. No red flags. A trial of therapy… success… save billions in unnecessary medical care. Very routine scenario in Allopathic based medicine. 45 years as a chiropractor. Basic health care advice… do the simplest things first and take the least medication possible. Just saved the country half a trillion or more annually. 😊